Our plans for the NHS, social care and communities for managing respiratory viruses.
Contents
Purpose
This publication sets out:
- the public health context as we move into the autumn and winter 2023 to 2024 season
- our approach to responding to respiratory viruses in Wales
Central to our approach is our objective to protect the most vulnerable in our society from serious illness. Infection Prevention and Control (IPC) measures remain a key component of practice to reduce transmission in health and care settings of COVID-19 and other infections, such as influenza, Respiratory Syncytial Virus (RSV), and norovirus.
The purpose of this publication is to:
- highlight priority areas of focus to help mitigate acute system pressures
- set out clear expectations of the health and social care system in responding to respiratory viruses
- set out how the Welsh Government will support the health and social care system to respond efficiently and effectively
- set out how we can prepare our communities for a potentially challenging autumn/winter
Context and modelling
We anticipate a seasonal rise in respiratory viruses over the autumn and winter, alongside further waves of COVID-19 infection.
We are also expecting to manage outbreaks through the arrangements we have in place under the outbreak control plan and monitoring of COVID-19 variants will continue including the emergence of BA.2.86. If there is a risk of higher transmissibility and severity, we will consider appropriate precautionary measures focused on protecting the more vulnerable including a higher level of infection and prevention control measures, more targeted testing, revising vaccination plans and issuing of stronger guidance to the public on measures they can take to protect themselves and others.
Influenza
Following a fairly constant, low level of influenza and pneumonia admissions from spring 2020 to summer 2022, the 2022 to 2023 winter season saw a peak in admissions approximately 1.5 times the levels usually seen before the COVID-19 pandemic. This was similar to one of the scenarios that we produced for winter 2022 to 2023 which was based on modelling by the University of Warwick which suggested the first ‘rebound’ influenza season after the pandemic could be 50-100% higher than a typical season. However, the actual total of admissions seen throughout the season was slightly lower than pre-COVID-19 levels. The peak dropped off rapidly in mid-December, which is similar timing to several of seasons seen before the COVID-19 pandemic but a more rapid drop-off in the epidemic curve than usual.
Scenarios for influenza and pneumonia are being produced for winter 2023 to 2024 which have the same type of influenza season as was observed pre-COVID-19, or a more severe influenza season. Influenza seasons are difficult to predict and vaccine uptake and vaccine match to circulating virus subtypes are important factors.
RSV
For RSV, total numbers of RSV admissions across the whole season returned to close to pre-COVID-19 levels in 2021 to 2022, although this wave came early. Last year (2022 to 2023) saw a split of activity with a smaller summer wave and a larger winter wave, but with total activity very similar to a pre-COVID-19 season. Currently RSV activity is low but we have scenarios of a split summer and winter wave similar to last year, and a single winter wave.
COVID-19
COVID-19 is also hard to predict. We have several different scenarios – last winter we saw two waves in rapid succession, a pattern which continued until around spring 2023, since when COVID-19 activity has been low, although increased slowly into August 2023. The level of hospital activity for COVID-19 will depend to an extent on vaccine booster uptake in vulnerable groups as well as the emergence of new variants – as of early September 2023, XBB1.16 remains the dominant variant, accounting for 37.6% of all sequenced cases but EG.5.1. is increasing as a proportion of cases. The newly identified variant BA.2.86 in late August has a high number of mutations and is genomically distant from both its likely ancestor BA.2, and from currently circulating XBB-derived variants. The variant is being monitored carefully but the impact is currently uncertain on transmissibility and severity. The emergence of BA.2.86 may also impact the central scenario for a winter similar to 2022 to 2023 as it may result in an earlier timing of a wave this autumn.
Combined pressures
Concurrent risks such as influenza, COVID-19, RSV, invasive group A streptococcal disease (iGAS), cold weather and industrial action occurring at once, as they did last winter, are very likely to place significant pressures on services. The most likely scenario peaks at around 150 combined admissions per day for COVID-19, influenza and pneumonia, and bronchiolitis due to RSV in winter 2023 to 2024 with peak occupancy around 1,000 -1,100 beds which is around 10-11% of the total number of hospital beds in Wales NHS.
Last year increases in illness due to strep A, which were amplified by media coverage of deaths due to iGAS, meant a large surge in activity around strep A symptoms. Other diseases like measles may see outbreaks this winter. There may also be concerns around avian influenza or other novel influenzas in humans.
We aim to publish further modelling to inform partners about these scenarios for winter 2023 to 2024.
Key actions
Surveillance
Effective and routine respiratory disease surveillance is an important feature of the health protection system in Wales. The intelligence we collect will help guide investment decisions and policy choices that will need to be made this winter.
Our aim is to deliver an effective combined surveillance system that provides timely information to aid effective risk assessment and risk management decisions to reduce harm from COVID-19 and other respiratory viruses.
Public Health Wales (PHW) is implementing an integrated respiratory surveillance plan, in line with principles of surveillance recommended by the World Health Organisation and the European Centre for Disease Prevention and Control. This considers the pandemic virus SARS-CoV-2 alongside other respiratory pathogens and assesses the impact of these pathogens at different levels from asymptomatic to severe hospitalised cases.
This surveillance involves multiple systems and routes of reporting, coupled with specialist microbiology and genomics and linked to other data such as vaccinations and hospital admissions. Where possible we will use existing data, enhanced by linkage and data science methods.
Work has been undertaken to integrate separate surveillance reports for COVID-19 and influenza into an integrated suite of outputs covering each level of disease severity and surveillance type. PHW will also develop collections of reports focusing on specific populations groups, starting with children.
A weekly interpretive summary (including a highlights of available international surveillance), covering key points from each surveillance system will be provided to Welsh Government. This will include:
- Community sentinel surveillance in GPs and community pharmacies.
- Severe Acute Respiratory Infection (SARI) surveillance in hospitals covering admissions and ICU beds taken up due to acute respiratory infections.
- Cause specific and seasonal all cause mortality data.
- Sequencing/genomics reports on SARS-CoV-2 variants and influenza clades.
- Vaccine uptake for COVID-19 and influenza.
- Vaccine equity reports relating to the COVID-19 autumn booster programme
- Data on other causes of acute respiratory infections, such as Group A streptococcus, mumps and pertussis.
In addition to the above, enhanced surveillance/evaluation will be undertaken on vaccine effectiveness, RSV and the burden of respiratory diseases.
To assure timely and accurate interpretation of our surveillance data we intend to continue to utilise local intelligence collected from our established professional networks. A number of national multi-disciplinary health and public protection groups will continue to meet regularly to consider local and regional intelligence.
We continue to have in place monitoring and oversight arrangements to review the surveillance data and intelligence on respiratory viruses. This builds on the approach adopted throughout the pandemic to combining a wider range of scientific evidence and analysis from different disciplines alongside local intelligence and surveillance.
Vaccination
Vaccination is a vital tool in helping to mitigate the effects of respiratory viruses circulating in the community, protecting the vulnerable and supporting the resilience of the NHS and care systems. Annual vaccination programmes targeting seasonal influenza have been a feature of healthcare in Wales for many years and have been slowly expanded in scope over that time. More recently, a programme of vaccinating against COVID-19 has been developed in response to the threat posed by the pandemic. While still developing and responding to change, the COVID-19 programme is becoming increasingly regularised and its scope refined.
Last autumn the first Winter Respiratory Vaccination Programme for Wales was delivered by bringing together the COVID-19 and influenza vaccination programmes. This enabled health boards to offer an improved experience for patients. Over 1.1 million people received a COVID-19 booster and over one million influenza vaccines were administered over the course of the programme. Nevertheless, despite this overall success, there was a decline in uptake amongst some eligible groups. For example, uptake in relation the childhood influenza programme has fallen year-on-year in recent seasons and there remained differences in uptake relating to socio-economic status and ethnicity as well as regional disparities.
For 2023 to 2024 the National Influenza Immunisation Programme and the COVID-19 booster programme will again be brought together to form a single Winter Respiratory Vaccination Programme (WRVP 2023 to 2024). This programme will be underpinned by the key principles of:
- protecting those at greatest risk
- protecting children and young people
- protecting frontline health and social care workers
- protecting the NHS
The WRVP 2023 to 2024, and in particular vaccine eligibility, will be guided by the latest clinical and scientific evidence and by the latest advice from the Joint Committee on Vaccination and Immunisation (JCVI) and the Chief Medical Officer for Wales.
The priority will be to maximise uptake of both influenza and COVID-19 vaccines for all those who are eligible. Health boards will be expected to redouble their efforts to ensure vaccines are easily accessible and to develop plans to reduce barriers which cause inequity.
For the WRVP 2023 to 2024, the following ambitions and expectations have been set out in respect of offers and uptake:
- a COVID-19 booster vaccine should be offered to all those who are eligible by 30 November 2023
- the influenza vaccine should be offered to all those who are eligible, at the earliest possible opportunity, and the uptake expectations are set out below
| Influenza | COVID-19 | |
|---|---|---|
| Frontline health and care workers | 75% | All frontline staff to be offered a vaccine at earliest opportunity |
| Other eligible adults | 75% | 75% |
Health boards are expected to reduce the gap in uptake rates between the least and most deprived communities within their health board area (against uptake levels achieved during the WRVP 2022 to 2023 programme).
Health boards will be expected to develop plans to reach 75% uptake for 2-and-3-year-olds, and in the schools-based programmes, by the end of the 2025 to 2026 season. Each health board is expected to be able to demonstrate the commencement of this improvement during the 2023 to 2024 season.
There will also be renewed focus in the WRVP 2023 to 2024 on the following groups:
2 and 3 year-olds
As well as protecting these very young children from serious illness, vaccination of this age group also helps to protect their carers, parents, grandparents and the wider community and reduce general levels of transmission.
Pregnant women
Will be encouraged to get vaccinated to help protect themselves and their babies. Evidence shows pregnant women have a higher chance of developing complications if they get influenza or COVID-19, particularly in the later stages of pregnancy.
Health and social care workers
Will be encouraged to take up the offer of the influenza vaccine as early as possible. The protection offered by vaccinations will help prevent frontline workers becoming ill and will also protect the resilience of the health and social care system from becoming overwhelmed.
COPD patients
Should be offered both vaccines at the earliest opportunity owing to the severe impact respiratory illnesses can have on these patients.
To implement the WRVP 2023 to 2024 effectively, health boards have been asked to plan for a single, coordinated, and coherent programme for both vaccines. Wherever possible, delivery models should be aligned to allow for co-administration, to help maximise efficiencies and reduce vaccination inequity. Health board plans will be expected to state how they will achieve the uptake and performance targets that have been set, through the governance of Vaccination Programme Wales.
Catch-up activity for children’s vaccinations – including MMR vaccination - has been under way over the summer months in an attempt to vaccinate those who have missed out over the past few years. It is hoped this will help ensure wider protection as we go into winter. At the same time engagement is being undertaken with school leaders to identify the barriers to uptake in school settings and to help overcome them.
Recent reductions in uptake amongst pregnant women will be tackled through engagement with midwives and the importance of health and social care workers taking up the offer of a influenza vaccine is being addressed through a renewed emphasis on it in communications with health boards and the social care sector and through all communications campaigns.
We will continue to review our vaccination programme during the autumn in response to the surveillance on respiratory viruses circulating including emerging variants.
Testing
Last winter, testing for COVID-19 and other respiratory viruses covered a range of settings. In addition to clinical management and supporting incidents and outbreaks, routine symptomatic testing was recommended for several cohorts. Over the summer, testing was focused on supporting clinical management of patients and identification of vulnerable individuals who would benefit from specific anti-viral treatment for COVID-19 or influenza, plus to support infection control activities and the management of incidents or outbreaks in closed settings.
The approach to testing this autumn and winter is based on the assumption that we expect to see a peak in respiratory viruses, but that at this time there are no firm indications these will be particularly severe. However, we will continue to closely monitor the emergence of the new BA.2.86 and any other COVID-19 variants that may cause significant health impacts, or if co-infection, for example with influenza, emerges as a major concern. If additional precautionary measures are needed, the testing strategy will be reviewed.
While we maintain our focus on protecting those who are most at risk of serious illness, for most people we continue to recommend that they should manage their symptoms without the need to test public health guidance for the general public | GOV.WALES.
For autumn and winter 2023 to 2024, testing is currently recommended as follows:
- For symptomatic individuals who are eligible for anti-viral treatments. This includes people in the community and/or in closed settings such as care homes, residential special schools and prisons.
- To identify and support the management outbreaks in closed settings.
There are also currently 3 programmes of active surveillance involving testing:
- SARI surveillance - Patients presenting to secondary care with acute respiratory illness – respiratory multiplex testing.
- GP Sentinel surveillance - Patients presenting to primary care with influenza-like illness – respiratory multiplex testing.
- Pharmacy surveillance - Individuals presenting to pharmacies with influenza-like illness – respiratory multiplex testing.
The testing of symptomatic health and social care staff is not routinely recommended (unless they are personally vulnerable and anti-viral therapy would be appropriate). Symptomatic staff should be excluded from work based on symptoms and follow the guidance Advice for health and care staff on respiratory viruses including COVID-19: guidance | GOV.WALES. Testing may be deployed as part of management of specific incidents.
Pre-admission screening to hospital is not recommended unless there is clear evidence that the there is an identified risk to an individual associated with concurrent planned treatment (such as chemotherapy) and infection with COVID-19.
Pre-admission testing for residents of nursing or care homes is not currently recommended as the risk of introduction of COVID-19 into such settings is significantly reduced due to high rates of immunisation.
However, we are closely monitoring the emergence of any new COVID-19 variants such as BA.2.86 and will revise this advice if additional precautionary testing measures are required.
Anti-viral treatment
Influenza
The National Institute for Health and Care Excellence (NICE) recommends the use of:
- antiviral medicines oseltamivir and zanamivir for the treatment
- and prophylaxis of influenza in adults and children over 1 year who are particularly at risk from influenza infection and who fall into one or more of the clinical risk groups defined and updated each year by the Chief Medical Officer (CMO).
Treatment can be prescribed by general practitioners (GPs) for people in an at-risk group who have influenza like illness but must begin within 48 hours of the onset of symptoms. It is a condition of prescribing that the CMO has notified GPs the influenza virus is circulating in the community; that it has been determined in accordance with a community based virological surveillance scheme that influenza is circulating in the locality in which the patient resides or is present or was present at the time that the virus was circulating; or there is outbreak of pandemic influenza.
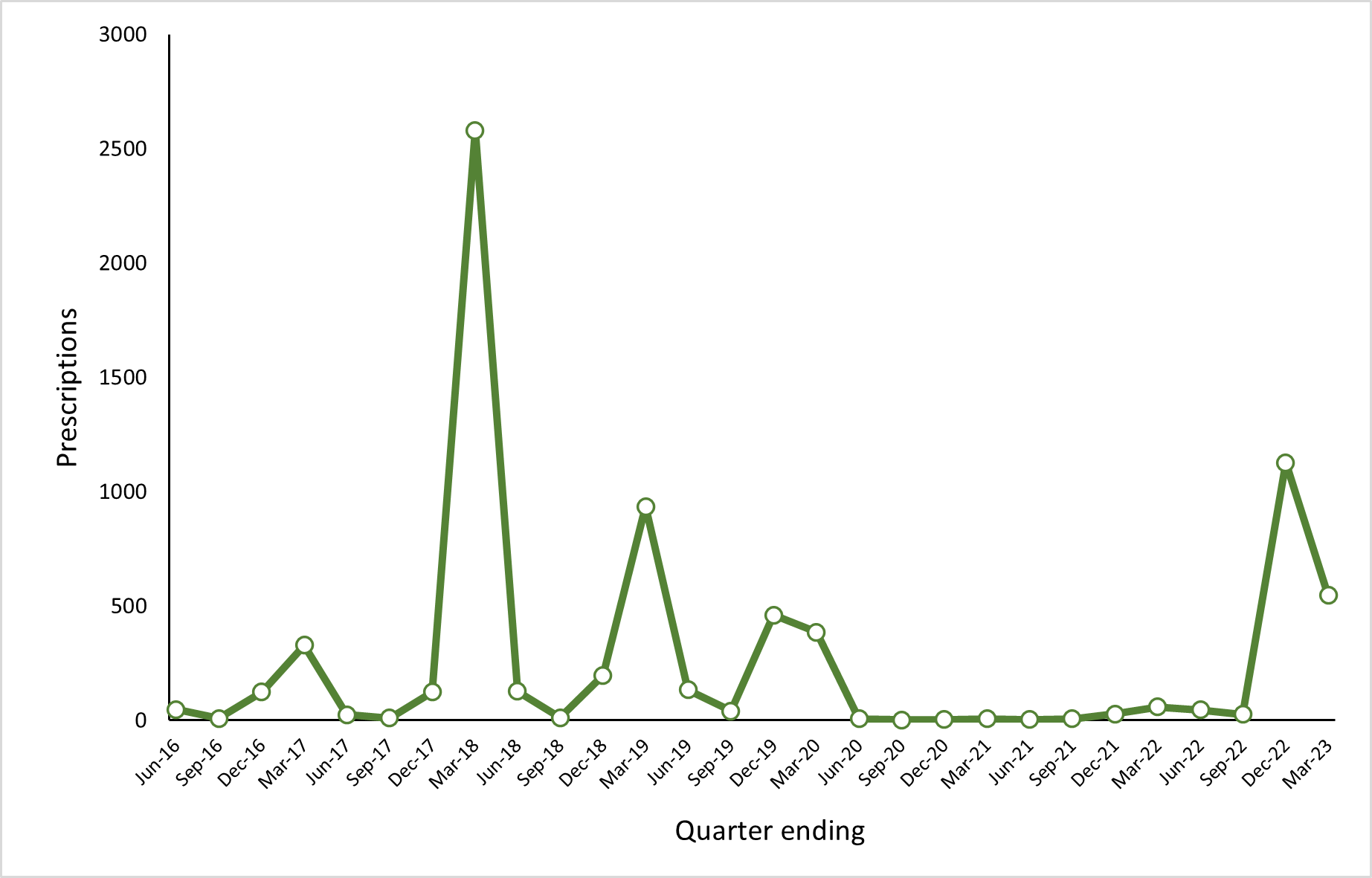
Prescribing patterns in primary care align closely to the incidence of influenza (figure 12) however there is a need for health boards to have arrangements in place which ensure sufficient supplies of influenza antivirals are available both for general prescribing for the treatment of influenza, and in larger quantities for prophylaxis necessary for the management of outbreaks in residential care establishments. We will take steps to facilitate the prompt prescribing of influenza antivirals by GPs including out of hours, with a particular focus on improving access for people living in residential care. Alongside this we will work with health boards to ensure that have robust arrangements for the supply of sufficient quantities of antivirals within the timescales required for them to be effective.
Figure 11. GP prescriptions for oseltamivir and zanamivir (all preparations) by quarter April 2016 to March 2023
COVID-19
The National Institute for Health and Care Excellence (NICE) recommends the use the antiviral medicine nirmatrelvir-ritonavir for the treatment of COVID-19 in adults who have an increased risk for progression to severe disease as defined by the higher-risk patients eligible for COVID-19 treatments: independent advisory group. The monoclonal antibody therapy sotrovimab is also recommended for treatment of COVID-19 in the same cohort but only where a patient has a contraindication to nirmatrelvir-ritonavir.
Currently treatment is provided by antiviral services in each health board. Treatment is dependent on confirmation of COVID-19 infection by positive Lateral Flow Device (LFD) test and should begin within five days of symptom onset. More than 6000 eligible people received antiviral or monoclonal antibody treatment in 2022 to 2023 (figure 12). COVID-19 antivirals are not recommended for prophylactic use.
Health boards are expected to maintain arrangements for providing COVID-19 antivirals to eligible people in the community and to have robust plans to increase capacity in the event of increased demand or any expansion to the eligible cohort over the winter period.
LFD tests have been made available to the eligible cohort through direct delivery ahead of the winter. In the longer term we are exploring plans to ensure testing continues to be available following the closure of United Kingdom Health Service Authority (UKHSA)’s home channel later this year. We are also considering what arrangements need to be in place to support improved access to oral antivirals in primary care from 2023 to 2024.
Figure 12. Eligible people treated for COVID-19 in the community by week December 2021 to March 2023.

Public health messages and communications
Individuals and the general public
Respiratory infections can spread easily between people. Enabling and promoting individual behaviours to protect ourselves, each other and particularly the more vulnerable can have significant benefits to reducing transmission of respiratory viruses. Continuing the protective behaviours which we have all become familiar with will help reduce impact of future waves of coronavirus, whilst also reducing the impacts from other respiratory infections.
The key message is to protect yourself, your family and others this winter by taking up the vaccination offer, if eligible and stay up to date with your COVID-19 and influenza vaccinations.
General protective behaviours include:
- get vaccinated
- stay at home if you’re unwell and limit your contact with others.
- maintain good hand hygiene
- wear a face covering in crowded indoor or enclosed places, including health and care settings
- meet others outdoors
- when indoors, increase ventilation and let fresh air in where possible
Our advice for people with symptoms of a respiratory infection is to:
- get plenty of rest and drink water to keep hydrated
- use medications such as paracetamol to help with symptoms; antibiotics are not recommended for viral respiratory infections because they will not relieve symptoms or speed up recovery
- stay at home and avoid contact with others until you no longer have a high temperature or until you feel better; you could ask friends, family, or neighbours to get food and other essentials for you
- work from home wherever possible; if you cannot work from home, talk to your employer about options
- if you've been asked to attend a medical or dental appointment in person, tell them about your symptoms
- tell people you have recently been in contact with that you're feeling unwell; this means they can be aware of signs or symptoms
- if you are concerned about your symptoms, they are worsening, or you can no longer manage at home, seek medical advice by contacting your GP or NHS 111; in an emergency dial 999
Key settings
Health
We know that winter 2022 to 2023 was very challenging, with peaks in respiratory illness and system pressures occurring earlier than usual, along with other concurrent risks such as industrial action and cold weather. We have also seen unseasonably high demand in paediatrics with pressures not receded over the summer months.
NHS Wales planning for winter is integrated into existing planning arrangements, which have been set out in the NHS Planning Framework for 2023 to 2026. This was released in autumn 2022 and planning started many months ago to ensure resilience throughout winter 2023 to 2024. Planning for seasonal peaks in demand across the system is a year-round exercise. System resilience for urgent and emergency care has been key to support improvements in hospital flow and discharges. There is a continued focus to reduce the instances of delayed transfer of care, increasing capacity in the system at peak periods and strengthening the support to improve discharge processes.
Those with respiratory illness are particularly at risk. This winter, NHS Wales will focus on the management of respiratory patients across Wales utilising the respiratory treatment toolkit and apply a number of respiratory disease national pathways (Chronic Obstructive Pulmonary Disease COPD, asthma, bronchiectasis, bronchiolitis, and RSV) to help people keep well and manage exacerbations to help reduce unnecessary admissions.
The cost-of-living crisis, increased energy costs and other pressures on people’s incomes also poses a risk, which can contribute to a difficult and disruptive winter. We will plan for this whilst recognising that pressure on services is much more extreme than we've seen prior to the COVID-19 pandemic.
The current Public Health Wales COVID-19 Infection Prevention and Control (IPC) Guidance sets out IPC measures to prevent transmission of COVID-19 in health and care settings in Wales. This guidance should be read in conjunction with the National Infection Prevention and Control Manual Wales, which includes guidance on the management of other winter viruses.
The patient testing framework sets out national guidance for testing, including for individuals on admission to hospital and care homes. The guidance is based on the best scientific, public health and expert evidence available but also recognises the importance for local decisions to be made about where or when testing may need to be increased or decreased depending on nosocomial rates, community transmission rates, or vulnerability of patients.
Vaccination programmes both for COVID-19 and seasonal influenza remain a critical part of our infection prevention and control plans. High levels of vaccination amongst the workforce both to maintain the health and wellbeing of our workforce, and to prevent onward transmission of infection to patients and colleagues. This will also help to maintain our staffing levels by minimising avoidable illness and so avoiding increasing the pressure on colleagues who remain in work. We will be working with social partners to encourage vaccination across our workforce.
In light of the emergence of BA.2.86 a systems letter was sent from the Chief Nursing Officer and the Deputy Chief Medical Officer to the NHS on 1 September noting the need to consider planning for a respiratory/infectious segregated pathway with the aim of limiting spread of infections and outbreaks within the admissions pathways when community rates are higher. It also referenced the importance of supporting vaccination for health and care staff, IPC guidance and that it may also be appropriate to re-introduce universal masking within these pathways and ensure that healthcare workers are fully trained in the use of their mask, face protection and other Personal Protective Equipment (PPE) in preparation for managing respiratory infections this autumn.
Social care
As we return to a business as usual status regarding COVID-19 we recognise that the risks posed are now reduced compared to the height of the pandemic but we continue to be vigilant alongside other respiratory infections. COVID-19 outbreaks in care homes were generally at a low level in 2022 to 2023, and deaths back to pre-pandemic levels indicating a positive impact of vaccination for those receiving care at home or within a care setting, and for care staff, as well as good adherence to infection prevention and control measures.
We’ll continue to promote PPE guidance and its adherence, with Welsh Government funding NHS Wales Shared Service Partnership (NWSSP)’s purchase and delivery of PPE to Local Authorities for re-distribution being extended to end of March 2024.
This autumn and winter we will continue to support social care including care homes and domiciliary care on infection and prevention control measures. This will include continuing to provide free personal protective equipment (PPE) and access to testing as set out above. In addition, we will continue to closely monitor outbreak data, vaccination uptake data and continue to engage with the sector over the autumn and winter to provide support where needed. A letter was sent to social care partners on 1 September setting out the importance of measures including infection and control and vaccination.
Visitors to care homes should be welcomed, encouraged and enabled when there is no outbreak at a care home. Visiting arrangements should be as open and flexible as possible. With regular asymptomatic testing being paused for social care settings, visitors will no longer need to take a Lateral Flow Test (LFT) before visiting a care home.
Any staff member who has symptoms of a respiratory tract infection including COVID-19 and/or has a high temperature is advised to stay at home and notify their employer as soon as possible.
When they no longer feel unwell and do not have a high temperature and are ready to return to work they may wish to discuss with their employer ways to minimise any risk as some may still be infectious. This may include undertaking a risk assessment if the staff member works with patients whose immune system means that they are at higher risk of serious illness despite vaccination.
Our ‘Further, Faster' work will continue to invest in community care to ensure additional clinical nurse specialists and health care support worker capacity is available over the winter period to support care closer to, or at home.
Education and childcare settings
The Education and childcare: coronavirus advice offers flexibility to determine what is required to manage risks. It remains important for education and childcare settings to consider what they can do to reduce the spread of respiratory viruses including COVID-19 and protect their learners and staff, including any additional protections for those who are more vulnerable. By continuing to implement public health control measures, schools and settings will help keep the spread of the virus low, improve public and staff confidence and minimise the potential of further disruption.
There is additional advice for staff and pupils of special educational schools, based on the objective of protecting the more vulnerable and reducing the risk of transmission to those who are at highest risk of adverse outcomes and within closed settings.
The Emergency planning and response guidance for education and childcare settings | GOV.WALES provides advice on how education and childcare settings should plan for and deal with emergencies, including significant public health incidents and severe weather.
Prisons
Health boards providing health services within prisons are expected to include prison health services within their own winter planning arrangements. PHW will continue to support through the production of surveillance reports to provide intelligence on incidents and outbreaks and will remain in close contact with each prison to support and advise as necessary.
Health boards will need to ensure sufficient resource is allocated to prison healthcare teams in remand prisons as these will need to keep up vaccination pace for the entire winter due to their rapid turnover of admissions.
Businesses and employers
We advise all businesses, employers and event organisers to continue to implement effective public health control measures. These will help protect workers, contractors, visitors and customers from exposure and prevent the spread of coronavirus. The most effective way of preventing the spread of any communicable disease in any premises is to prevent the virus being present in the first place.
Employers should consider what action they should take if a staff member is displaying any symptoms of a communicable disease (such as influenza, COVID-19 or norovirus) or have tested positive for coronavirus. What is reasonable will depend on a number of factors, including whether it is feasible for the work to be carried out from home.
Wherever possible, Welsh Government would encourage employers to discuss and agree any changes to absence management with the workforce and with trade unions prior to any changes being implemented.
Winter communication campaign
PHW has been commissioned to deliver a high-profile campaign to encourage preventative behaviours for respiratory viruses this winter, based on agreed behaviours and audience insight. The campaign will be designed to be flexible to respond to emerging threats and issues and will target a broad range of the population focusing on increasing knowledge and motivation for the public to adopt preventative behaviours over winter when there is an increased risk of spread. It will focus on creating social norms and everyday routines to help us stay well and reduce rates of mortality and morbidity. PHW will engage with the wider NHS to ensure messages are consistent across Wales and materials shared.
Alongside and aligned with the preventative behaviours campaign will be the Winter Respiratory Vaccination Campaign. It will promote the COVID-19 autumn booster and influenza vaccination to eligible audiences in Wales. The campaign will run until December 2023, with mop up activity taking place in January/February 2024. The vaccination campaign will include key messages targeted around the adult influenza and COVID-19 vaccines, health and social care workers, children’s influenza programme and pregnant women.
