National framework for social prescribing
A description of social prescribing in Wales and a plan of how to provide it throughout the country.
This file may not be fully accessible.
In this page
About this document
This document sets out the Welsh Government’s programme for government commitment for an NFfSP. It has been developed following a period of engagement with over a 1,000 stakeholders and responds to our consultation exercise which explored a number of key themes.
It is structured into 5 sections.
Section 1: introduction and background
This section provides a definition of social prescribing in Wales, explores the potential benefits of social prescribing and summarises the available evidence base.
Section 2: context
This section provides the legislative and strategic context for the NFfSP in Wales, provides information on the actions people can take to support their health and wellbeing and sets social prescribing within the spectrum of support needed to enable people to take action.
Section 3: development of social prescribing in Wales
This section describes how social prescribing has grown across Wales in recent years and highlights key pieces of research. It also sets out the current landscape in Wales and how the NFfSP was developed.
Section 4: the model of social prescribing in Wales
This section provides clarity around the model of social prescribing in Wales.
Section 5: National Framework of Social Prescribing (NFfSP)
This section sets out the core objectives of the NFfSP and its cross-cutting themes, the guidance and tools supporting the framework and sets out how we will drive forward the future development and implementation of the NFfSP.
Foreword by the Deputy Minister for Mental Health and Wellbeing
There are things we can all do to improve our health and wellbeing and many people are already able to access the many fantastic resources we have within our communities.
However, this can be difficult for some, and this is where social prescribing can help, and why, I am delighted to set out our plans for a National Framework for Social Prescribing (NFfSP).
Social prescribing is an umbrella term that describes a person-centred approach to connecting people to local community assets. It can help empower individuals to recognise their own needs, strengths, and personal assets and to connect with their own communities for support with their personal health and wellbeing.
Social prescribing across Wales is not new. The principles of social prescribing are woven into the very fabric of what Welsh Government does in terms of empowering people and communities, with the development of a national framework, a key programme for government commitment.
Our health and social care Regional Integration Fund (RIF) directly supports the development and delivery of integrated care which includes direct investment in social prescribing.
In 2022, we ran a consultation exercise to seek views on a Welsh approach to social prescribing which received over 190 responses, the feedback from both organisations and individuals has been extremely valuable and has directly shaped the development of the NFfSP.
I would like to take this opportunity to thank the many individuals and organisations who responded to the consultation exercise and worked with us to shape our plans and in particular the members of my task and finish group.
Social prescribing interventions have grown organically across Wales, with individual contracted providers, clusters involved in health and care, third sector and statutory organisations developing different delivery models.
This approach is welcomed as services must be delivered to meet local population need. However, our consultation exercise has told us that, there has been a lack of standardisation and consistency in the approach to social prescribing. This has resulted in confusion on the benefits it can offer amongst both the public and the workforce who deliver or encounter social prescribing. Communication between sectors, professionals and the public has also been impaired by this.
To provide reassurances on the consistency and quality of delivery across Wales and to respond to the issues raised as part of the consultation exercise, our NFfSP outlines the preferred model of social prescribing in Wales, helps to develop a shared understanding of the language used to describe social prescribing, and seeks to ensure consistency of delivery regardless of the setting. It does not intend to dictate how social prescribing is delivered in different communities, rather it will support its growth by setting out effective, high-quality standards across a connected system.
Lynne Neagle MS, Deputy Minister for Mental Health and Wellbeing.
1. Introduction and background
1.1 What is social prescribing?
Social prescribing is an umbrella term that describes a person-centred approach to connecting people to local community assets. Community assets include community groups, interventions and services which could be delivered online or in person, as well as buildings, land or even a person within a community.
Social prescribing is a way of connecting people, whatever their age or background, with their community to better manage their health and wellbeing. It can help empower individuals to recognise their own needs, strengths, and personal assets and to connect with their own communities for support with their health and wellbeing.
To help bring social prescribing to life, quotes from case studies gathered by Public Health Wales are included throughout this document..
1.2 Why social prescribing is important?
Expectations of social prescribing are high with it being considered as one of the solutions to:
- improving health and wellbeing of individuals
- reducing inequalities
- mitigating the impact of social determinants on health;
- and supporting recovery from the adverse effects of COVID-19 [footnote 1].
Though the benefits of social prescribing are wide-ranging, improved physical, mental and social wellbeing are commonly reported. This encompasses aspects of psychosocial health [footnote 2], healthy lifestyles and behaviours, social engagement, and self-management of long-term conditions [footnote 3].
Indeed, connecting people to their community may have a wide range of benefits, for example, we know that people who are lonely or socially isolated are at greater risk of, of being inactive, heart disease, stroke and high blood pressure and premature death. They are also more likely to experience depression, low self-esteem, sleep problems and an increased response to stress.
There is also a link between health and wellbeing and employability. There is potential for social prescribing to help people secure employment by creating opportunities to improve health and wellbeing; improve skills, confidence and networking; and directly support people to access volunteering opportunities and organisations who can help navigate job application processes. Similarly, connecting people to community assets which offer financial and housing advice could help ease financial concerns.
A person that has experienced financial and mental health concerns:
“Initially it was a food parcel: they delivered that straight away. They asked a little bit more about my situation and gave me the leaflet. I explained about my housing situation…They offered if I needed any clothes or anything like that. They were very helpful.”
By helping to strengthen community connectedness and cohesion there may be benefits to the wider community, a key factor in our Compassionate Cymru vision “to be a compassionate and caring nation that comes together to develop compassionate approaches to support people’s health and wellbeing”. Our Trauma Framework also advocates for a societal approach to understanding preventing and supporting the impacts of trauma and adversity.
It could also give people a more meaningful connection with nature and an appreciation of the role of culture in supporting their wellbeing, making them value community assets even more. Similarly, connecting with opportunities to be physically active provides multiple benefits to physical health and mental wellbeing, and could provide opportunities for stronger community cohesion.
A community asset outdoor project manager, Gwynedd:
“We’ve got a walking group, and there’s a guy on there who didn’t believe he could walk and just walked a very small amount of time…The woman running that programme is ace, and she’s just been encouraging him and being playful. Now he walks a couple of miles every time he does it, and him and his friends that he’s met through that programme have started a walking group.”
In addition, social prescribing can present an established route for individuals who may not engage with mainstream services or otherwise face stigma to re-enter the community, for example, those who have experienced homelessness or substance misuse. Re-introduction of people from stigmatised groups also raises awareness of recovery and could diminish the negative perceptions of people with substance misuse or mental health issues.
1.3 Current evidence base for social prescribing
Given that estimates show around 20% of patients consult their GP for what is primarily a social problem [footnote 4], the potential for social prescribing to reduce impact on frontline services is evident if alternative routes are more easily and widely available.
There is variable evidence in support of social prescribing, including:
- social prescribing reduces the footfall to GP surgeries by 15% to 28% [footnote 5]
- an average 28% reduction in demand for GP services following a social prescribing referral [footnote 6]
- results ranged from 2% [footnote 7] to 70% [footnote 8] reduction in unnecessary GP visits
- Reduction in people using general practice, with a reduction of 25% in appointments [footnote 9]
Furthermore, findings from the evaluation of the Rotherham Social Prescribing pilot pointed to an overall trend of participants’ reduced use of hospital resources before and after social prescribing. These included: inpatient admissions reduced by as much as 21% and accident and emergency attendances reduced by as much as 20% [footnote 10].
The evidence varies so much because the impact of social prescribing depends on the type of model used, the social prescribing practitioners and their backgrounds, the locality, and the assets available within the community [footnote 11].
National Institute for Health and Care Excellence (NICE) guidelines for the management of patients with two or more chronic conditions, emphasise the importance of non-pharmacological treatments and engagement in social activities [footnote 12]. A systematic review of 40 studies of social prescribing carried out in the UK found a range of benefits reported by participants and referrers.
These include: increases in self-esteem and confidence, sense of self-control and empowerment; improvements in psychological or mental wellbeing; reduced anxiety and depression [footnote 13].
A review of 24 studies reported that stakeholders such as GPs and patients perceived that social prescribing improved patients’ mental wellbeing and reduced their health service use, although there is limited quantitative evidence to support this [footnote 14]. A study of 342 participants on a social prescribing scheme in northern England found improvements in wellbeing and increased levels of health and social connectedness [footnote 15]. Reduced levels of loneliness were also found in an evaluation of a British Red Cross-delivered social prescribing service in the UK, where 72% of participants reported that they felt less lonely after receiving the support [footnote 16].
Within the British Medical Association plans for general practice to be carbon neutral within 10 years, social prescribing is identified as having the potential to improve patients health and wellbeing whilst also reducing GP practice attendance and use of the wider NHS.
There is also a growing body of evidence that undertaking nature-based activities can provide multiple benefits for health and wellbeing [footnote 17]. A systematic review of 143 studies found that ‘greenspace exposure’ is associated with a wide range of health benefits. These include: statistically significant reductions in diastolic blood pressure, salivary cortisol and heart rate and statistically significant reductions in the incidence of diabetes, all-cause and cardiovascular mortality [footnote 18]. An emerging evidence base indicates that connecting with others in nature can increase feelings of connectedness with others and lower participants’ stress levels [footnote 19]. Although the exact pathways via which contact with nature may lead to health improvements are not known, possible pathways may include: air quality, physical activity, social cohesion and stress reduction [footnote 20].
The majority of the evidence base for social prescribing to date is centred on the impact on the health system, although as indicated there are potential benefits to many parts of society. As part of monitoring and evaluating the impact of the NFfSP, it is the intention to develop a wider evidence base than currently exists.
2. Context
2.1 Legislative and strategic context
The principles of social prescribing, such as taking an early preventive approach to enhancing people’s health and wellbeing, addressing health inequalities and strengthening community cohesion, are consistent with the Social Services and Well-being Act (Wales) 2014, the Well-being of Future Generations Act (Wales) 2015, and our long term plan for health and social care ‘A healthier Wales’.
It is woven into the very fabric of what Welsh Government does in terms of empowering people and communities, whether it’s part of the National clinical framework, the six goals for urgent or emergency care; together for mental health, or connected communities our strategy to tackle loneliness and isolation.
Our 'Programme for government 2021 to 2026' commits to introducing an all-Wales framework to roll out social prescribing to tackle isolation, whilst recognising the breadth of potential for many more health and wellbeing benefits go beyond tackling isolation.
2.2 Factors influencing our wellbeing
Preventing ill health and promoting good wellbeing is vital. The factors influencing our physical, social and mental wellbeing can be complex. However, we know from the evidence base [footnote 21] that there are activities we can undertake to protect and improve our wellbeing to help us cope through difficult times and to flourish when times are good.
The activities people engage with will be unique to each individual, but there are common themes including:
- connecting with people and developing trusted relationships
- moving more and being physically active
- finding ways to be creative
- engaging with nature, culture and heritage
- learning something new or making time for hobbies
- helping others and volunteering
- finding time to relax and, for babies, children and young people, time to play [footnote 22]
- good quality sleep
Our ability to access these protective factors and resources will of course vary by context and circumstances.
Many of these activities can be interconnected, for example joining a local outdoor walking group can help us feel part of a community and well as providing an opportunity for physical activity and a chance to engage with nature. We often connect with people with similar interests and experiences, so doing activities we enjoy as part of a group can help us form social bonds. It can also help us to meet new people and people with different experiences, helping to build a wider sense of community.
Additionally, engaging with activities individually, particularly those that help us achieve a sense of “flow” (where we’re so engaged with an activity we lose sense of time), can help us to regulate our emotions.
People should be enabled to seek advice and support for specific concerns for example, bereavement, money worries caring responsibilities or housing concerns.
There are lots of community assets which may help boost health and wellbeing across Wales. For example, in libraries, community centres, health and care centres, sport clubs and leisure centres, art and cultural groups. However, people may not always know how to find and take part, may not have the confidence to take part, or be restricted by geographical or physical boundaries. We want to challenge this and ensure everyone has access to community assets. Social prescribing is a key tool to enable this.
2.3 Empowering people to take action to support their own health and wellbeing
Often, people will have the confidence and ability to recognise opportunities and act themselves to support their own health and wellbeing. Or they may be prompted and supported to do so by family members and friends.
However, whilst people can and should be empowered to directly access community assets to support their health and wellbeing, it is recognised that a spectrum of support is required to enable effective behaviour change so that people can engage in activities and access the interventions or services they need. This is illustrated in the diagram below (figure 1). The level of support a person needs will vary over a person’s lifetime and be dependent on the circumstances people find themselves in and how we behave towards people seeking support is crucial.
Figure 1.

As shown in the diagram, people are often prompted to act following contact with a health or other professional who provides advice, signposting or referral to a specific community asset they feel may be beneficial.
‘Making every contact count' [footnote 23] is an approach to behaviour change that utilises the millions of day to day interactions that organisations and individuals have with other people to support them in making positive changes to their physical and mental health and wellbeing.
In other circumstances, dedicated wellbeing support is needed to enable behaviour change such as the help me quit [footnote 24] stop smoking programmes, allowing for a much more detailed discussion between the individual and the professional. As the model for social prescribing in section 4 demonstrates, social prescribing also involves dedicated time for a detailed discussion to understand ‘what matters’ to an individual and to develop a person-centred action plan.
Finally, it is recognised that where people have more complex clinical or social care needs, these may need to be met through statutory healthcare or social care services for example a substance misuse service.
3. Social prescribing in Wales
3.1 Development of social prescribing in Wales
Social prescribing has grown in an organic way across Wales with awareness and implementation growing over time.
The development of social prescribing in Wales
2016: Programme for government commitment to run mental health social prescribing pilots.
2017: Senedd plenary debate on social prescribing.
2017: Evidence map and narrative summary published.
2018: Launch of Wales Social Prescribing Research Network (WSPRN).
2018: 'Social prescribing in Wales' published.
2019: Connected communities strategy for loneliness and isolation includes national actions on social prescribing.
2020: WSPRN becomes the Wales School for Social Prescribing Research (WSSPR).
2021: Programme for government commitment to develop a National Framework for Social Prescribing (NFfSP).
2021: Welsh Parliament research briefing published.
2021: 'Understanding social prescribing' in Wales published.
2022: Social prescribing interface paper published.
2022: Consultation exercise on NFfSP launched.
2023: NFfSP published along with explainer video, glossary of terms, competency framework.
2024 onwards: remaining components of NFfSP will be published and implementation of NFfSP monitored.
3.2 Reports referenced in the timeline
In 2017, the Public Health Wales Observatory Evidence Service published the social prescribing evidence map and narrative summary.
A report published in 2018 by the Primary Care Hub in Public Health Wales on ‘Social prescribing in Wales' mapped the progress being made in developing social prescribing services across health board areas.
Understanding social prescribing in Wales: a mixed method study was published in 2021. The study undertaken by Public Health Wales, University of South Wales, Data Cymru and the Wales School of Social Prescribing Research (WSSPR) aimed to outline the baseline from which a national framework could be developed, including an understanding of the interactions between service users and social prescribing projects, the social prescribing workforce in Wales, and also the impact of the COVID-19 pandemic.
A Senedd research briefing into social prescribing was also published in 2021 which examined what social prescribing is, how it is being used and the role it may play in improving health outcomes
A social prescribing interfaces (2022) paper published by the Primary Care Hub in Public Health Wales highlights the synergies and distinctions between physical and mental health services; wellbeing activities and community assets; and social prescribing. The social prescribing interfaces model reflects the distinctive ways that people engage with these services and activities, but recognises the clear meeting points when viewed together.
3.3 Current landscape of social prescribing in Wales
The baseline study [footnote 25] referenced in section 3.2 provided a snapshot of what we understand currently about social prescribing in Wales.
Figure 2: Number of individuals referred to and using social prescribing services in Wales, by year.
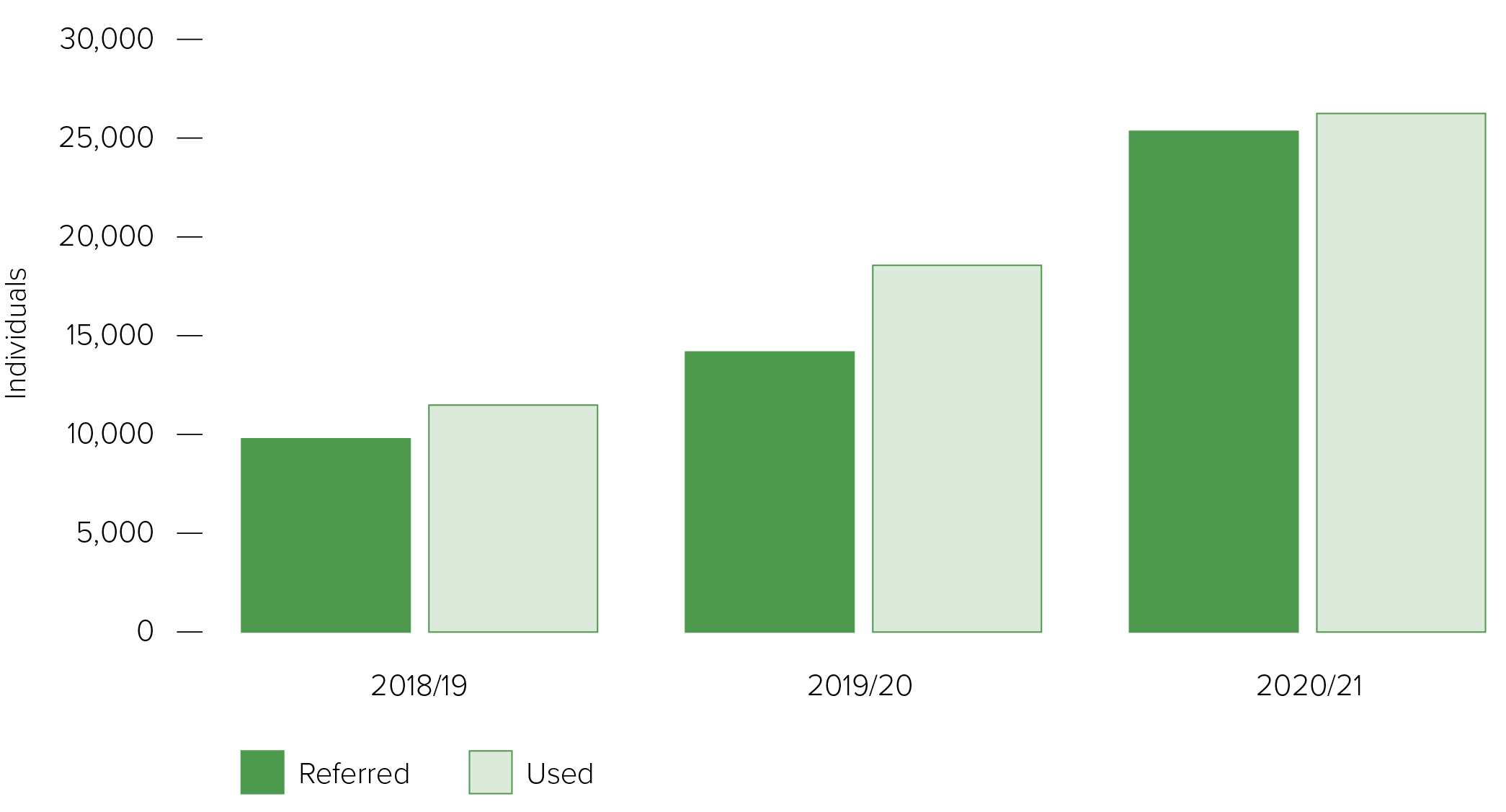
Source: Social Prescribing Activity in Wales, by Data Cymru.
The study showed there had been a clear year on year increase in referrals and use of social prescribing over the last three years from around 10,000 in 2018 to 2019 to just over 25,000 in 2020 to 2021.
Figure 3: Total number of organisations that provide a social prescribing service in each local authority in 2018 to 2019.
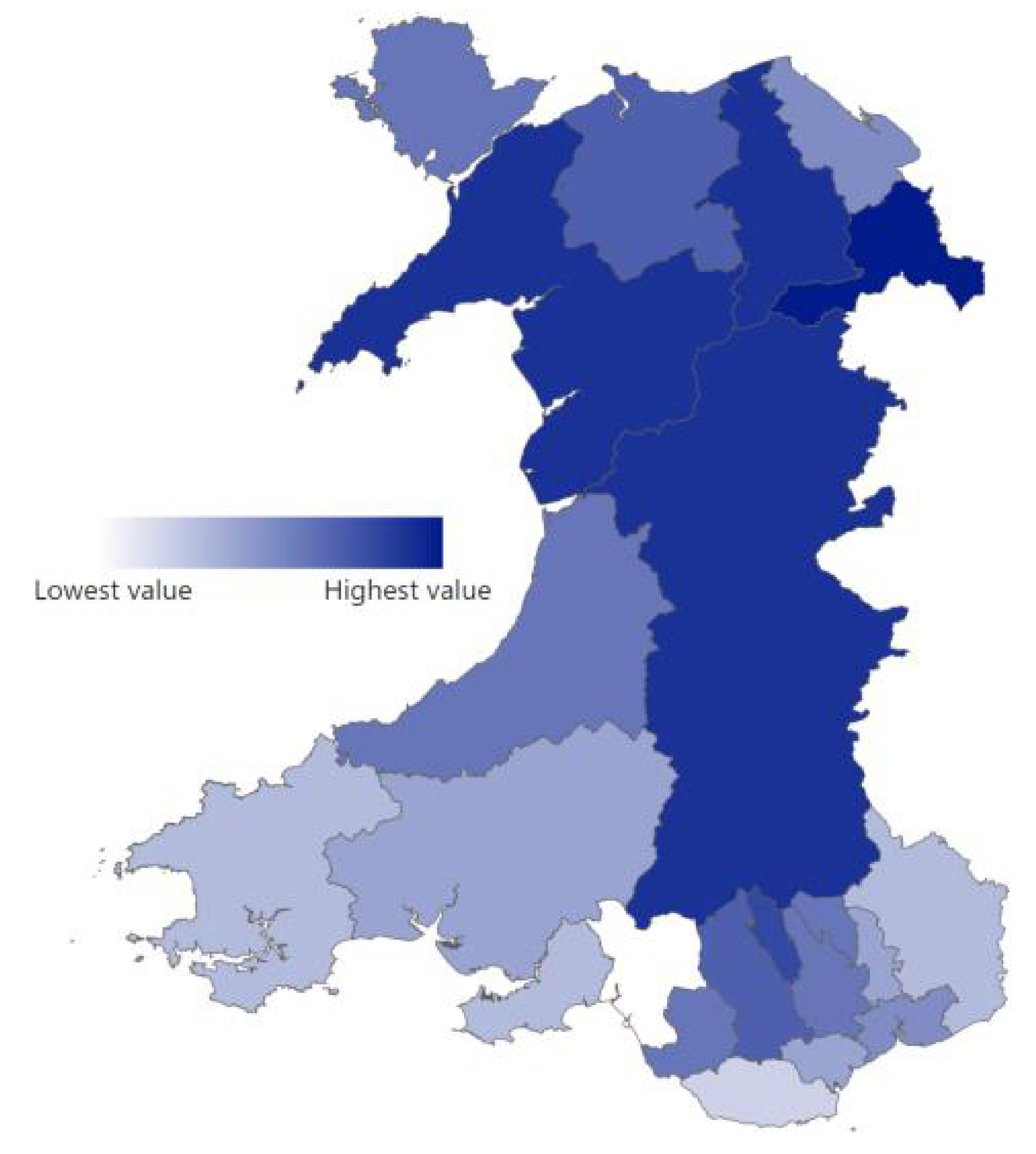
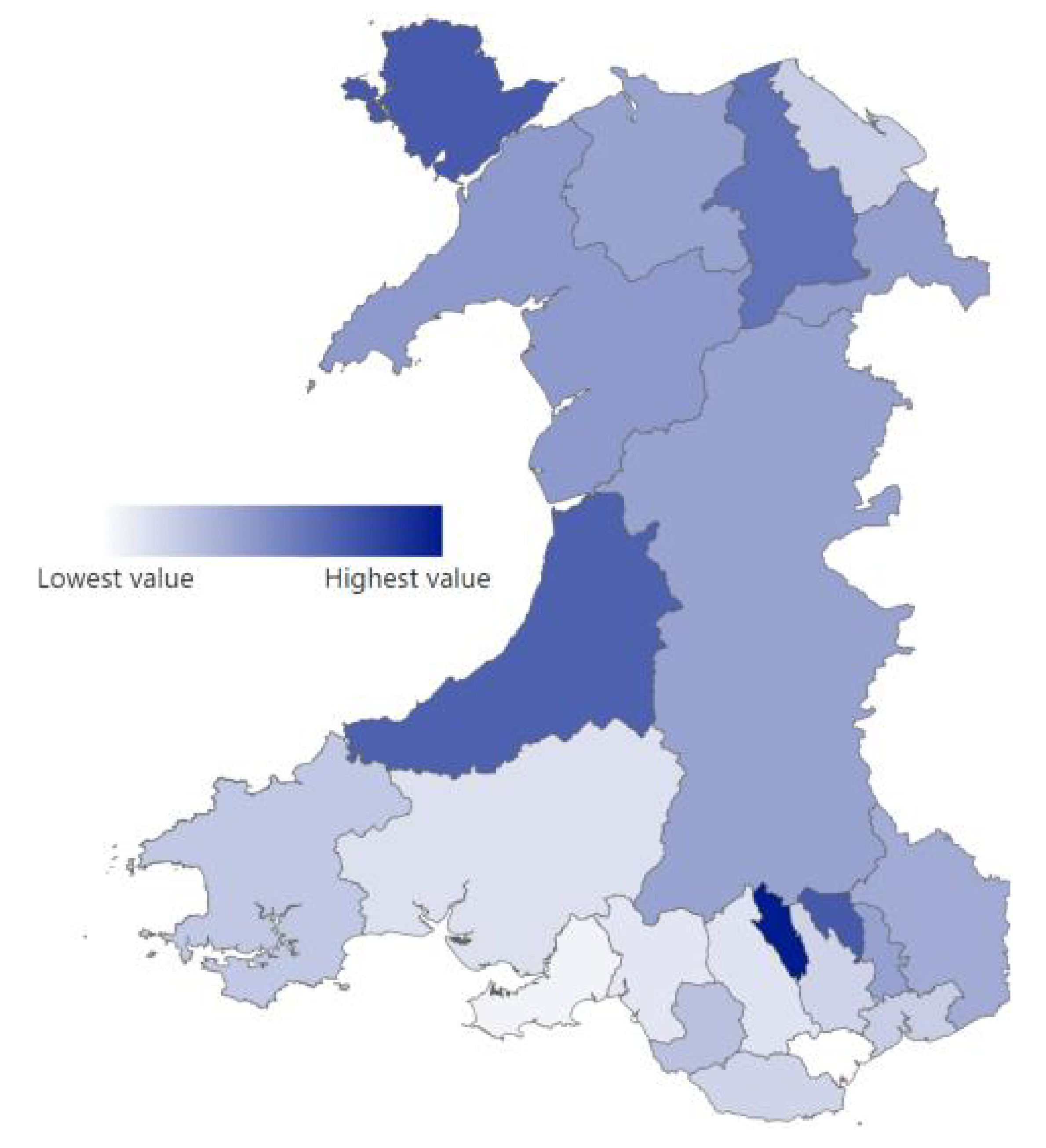
Figure 4: Number of organisations that provide a social prescribing service in each local authority, per 100,000 of the population in 2020 to 2021.
The number of organisations within each local authority providing data on social prescribing varied, with Wrexham reporting the highest (19) and Neath Porth Talbot the lowest (9).
Merthyr Tydfil had the highest number of organisations providing social prescribing services per 100,000 of population, whilst Cardiff reports the lowest in Wales.
Most organisations that responded were representative of the third or voluntary sector, and local authorities. Other organisations that responded identified as either healthcare providers, housing, universities, or wellbeing centres or hubs.
A community hub manager, third sector, Conwy said:
We have a lot of people moving into the area to retire…People become very isolated. It’s trying to build those networks in place before that happens. That’s the important thing: building that sense of community.
3.4 How the National Framework for Social Prescribing (NFfSP) has been developed
A task and finish group, chaired by the Deputy Minister for Mental Health and Wellbeing was established to oversee the development of the NFfSP. A list of organisations who participated in the task and finish group can be found in Annex A.
To support and inform the development of the NFfSP, a logic model was produced which identifies the long-term outcomes that it aims to influence at individual, community and system level [footnote 26].
These outcomes are holistic and demonstrate the potential benefit of social prescribing at a population level, including impacts on wider determinants of health.
The findings from the baseline report and other research into social prescribing; alongside the expertise of task and finish group members; and engagement with almost 1,000 stakeholders, helped develop a person centred model for social prescribing in Wales and highlighted a number of key themes which were tested as part of a consultation exercise.
The consultation, which ran 28 July to 20 October 2022, received over 190 responses, which together with feedback received via online stakeholder events held during the consultation period, is captured within the ‘consultation report’.
Social prescribing long-term outcomes
- Improved population mental wellbeing and reduction in overall prevalence and inequalities within mental ill health.
- Improved population physical wellbeing and reduction in overall prevalence and inequalities within physical ill health.
- Improved population social wellbeing and reduction in overall prevalence and inequalities within poor social wellbeing, loneliness and isolation.
- A system impact on the wider determinants of health.
- Improved community wellbeing.
4. The model of social prescribing in Wales
Within Wales, organisations offering social prescribing are not just located in health care settings, rather they are based in a range of organisations. For example, GP surgeries, third sector organisations, housing associations, local authorities, or educational settings.
Person centred: at the heart of the model is the individual accessing social prescribing. Most social prescribing services in Wales are usually targeted at adults aged 18 years and over. However, whilst the adoption of social prescribing is not as common with children and young people, it is recognised that a life course approach is appropriate in social prescribing and there are opportunities to expand its use with people under 18.
Individuals may engage with community assets to help manage a broad range of health and wellbeing concerns such as, and not limited to, anxiety, loneliness, social isolation, chronic health conditions, bereavement, adopting healthy lifestyle choices or financial difficulties.
Often the issues people face are multi-faceted. An example of this could be someone who may have been bereaved and struggling with financial, practical, and emotional matters, requiring help with benefits advice and bereavement support; or someone with a recent diagnosis of cancer who may need additional social support alongside medical intervention.
A social prescribing project manager, Young People Service, Cardiff and the Vale of Glamorgan said:
It’s… really important to us that this is a working relationship with the young person: it isn’t telling them what to do, it’s working together. Often that’s managing expectations of what this looks like and what they can expect from us [and] what we can expect from them.
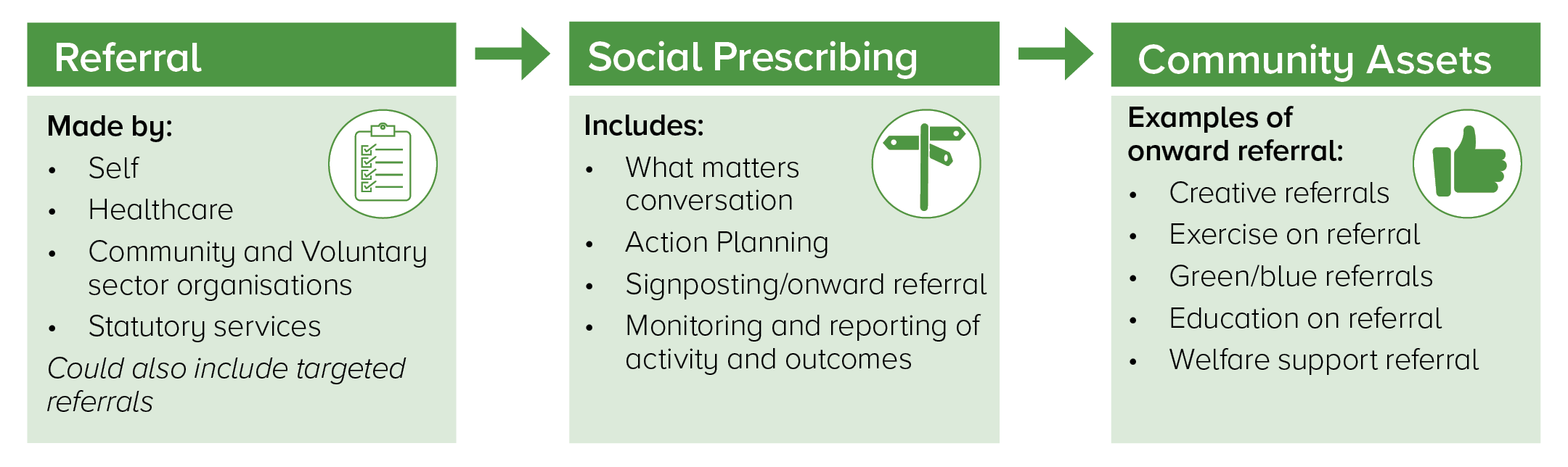
Social prescribing requires multiple organisations to work together to ensure a coherent, seamless social prescribing pathway.
Figure 5: The social prescribing pathway.
A frailty nurse, Cwm Taf Morgannwg Health Board area said:
We were trying to identify patients at risk of fuel poverty and around 1 in 10 patients that participated in the project were signposted to a warm home service but a much larger number had unmet health needs (1 in 5).
Sources of referrals into an organisation offering social prescribing are cross-sectoral and not limited to healthcare. For example, referrals can originate from community and voluntary sector organisations, statutory services and also includes self-referrals.
A GP, a referrer to social prescribing services, Cardiff and Vale University Health Board area said:
Previously, we would see patients with a lot of these problems, which we didn’t really feel equipped to help and support with. Medication isn’t necessarily going to help with those problems. I feel it’s really empowering to help us as GPs to support our patients in the whole of their lives. That in turn obviously improves health outcomes as well.
An organisation offering social prescribing may also proactively contact individuals or populations who have a specifically identified need. This is called targeted referral, examples of this approach may include individuals who are on waiting lists, individuals with chronic health conditions, or patients within a specialist service such as a ‘cancer unit’.
Social prescribing practitioners include those who practice social prescribing as their main role and those who practice social prescribing as part of their role.
Social prescribing practitioners can be employed by a range of different organisations, such as universities, local authorities, health boards or community and voluntary sector organisations. They may also be known by a variety of terms specific to the organisation in which they work. For example, link worker, community connector or wellbeing coordinator. Within Welsh speaking communities the term ymarferydd presgripsiynu cymdeithasol is commonly used.
A person that is a carer for their mother said:
I think I was just feeling a bit overwhelmed…a friend of mine noticed that I’m just not myself… things were getting to me, little things, and worrying about things that wouldn’t have got to me before. It was all just building up and building up.
[Social Prescribing Practitioner]…linked me in with the carer’s support project whereas I don’t think I would have taken that initiative and made contact. I might have taken a leaflet or a link, thought about it and then time would’ve passed, and I wouldn’t have got around to it.
A social prescribing practitioner will help facilitate change by holding a ‘what matters’ conversation with the person accessing the service. Together they will co-produce a person-centred action plan for them to engage with wellbeing activities, interventions and services, through signposting and referral into a wide range of community assets. The length of time a social prescribing practitioner spends with someone will vary depending on the scope of their practice, local arrangements and the needs of the individual.
The action plan could consist of several onward referrals to a range of community assets. Examples of onward referrals include:
- creative referrals
- exercise on referral
- green referrals
- blue referrals
- books on referral
- education on referral
- welfare support referrals
- buddy system
A person that cares for their partner who is living with dementia, Cwm Taf Morgannwg University Health Board area said:
[The Social Prescribing Practitioner] was very aware of the services available in the area. They gave me all the information that was available. We discussed what the different groups were, what I thought [partner] would be open to trying, and also what is available to me to give me advice, help, and respite.
Social prescribing practitioners will undertake ongoing monitoring and reporting of activity and outcomes and provide feedback to the original referrer if required.
A full range of sustainable community assets are crucial. However, it is inevitable that these may grow and decline depending on funding, demand and changing needs.
Organisations offering social prescribing are well placed to identify gaps and unmet needs and to feed this information into future commissioning plans and service design. This will help enable a joined-up approach to developing community assets.
It is important for social prescribing practitioners to spend time building relationships with the people and organisations who refer into their service, the people using the service, and the community assets available, to ensure their pathways runs smoothly.
An explainer video has been developed to set out the preferred model in Wales.
A community navigator team leader, South East Wales said:
It’s really about that network building: knowing who’s out there and supporting those groups…my colleague…supports groups to develop from the ground up. As navigators, the team can identify gaps or see things that are working really well and maybe if they could be fitted into another community.
5. National Framework for Social Prescribing (NFfSP)
5.1 Core objectives of the NFfSP
Social prescribing has seen a period of growth and development over the last decade. However, within Wales, as in other countries, there has been a lack of standardisation and consistency both in the terminology associated with social prescribing and in the model adopted. This has resulted in confusion on the benefits it can offer amongst both the public and the workforce who deliver or encounter social prescribing. Communication between sectors, professionals and the public has also been impaired by this.
The NFfSP sets out to describe the preferred model of social prescribing in Wales, help develop a shared understanding of the language used to describe social prescribing, and seeks to ensure consistency of delivery regardless of the setting.
The NFfSP will consist of a number of guidance documents and tools which have or will be coproduced with stakeholders across Wales, including Public Health Wales, Health Education Improvement Wales, the Wales School for Social Prescribing Research, Wales Council for Voluntary Action and representatives from delivery partners and providers.
A student support navigator in a university setting in North Wales said:
We’ll stay engaged with that student to make sure that support is working for them…or if we need to look at an alternative…We follow them through that journey to make sure they’re engaged and that it’s worthwhile for them, then…we can review and reflect with them then and look at what they’ve learnt from that process and how in the future they can support themselves to build resilience and encourage that empowerment
It does not intend to dictate how social prescribing is delivered in different communities, rather it seeks to support its growth by setting out effective, high-quality standards across the ‘whole system’.
Its core objectives are to:
- develop a shared understanding of the language used and the approach taken to deliver social prescribing in Wales
- support the social prescribing workforce and drive up knowledge and skills
- ensure quality of provision by community assets
- monitor and evaluate the development of social prescribing as it continues to grow across Wales
- improve outcomes for individuals; organisations, commissioners and referrers
An overview of the core objectives of NFfSP can be seen in Figure 6.
Figure 6. Core objectives of NFfSP.

5.2 Cross cutting themes
There will be cross cutting themes across the NFfSP, highlighting the importance of:
- Addressing inequality and inequity: for example, the Competence Framework for Social Prescribing Practitioners in Wales includes the impact of social inequalities on health; working in a culturally competent way that values diversity; equality and inclusion; respecting the beliefs, practices and lifestyles of people who use social prescribing services; and how these may affect their experience of the service; the planned national specification will also include the requirement to target currently underserved groups and the national standards will consider barriers to access.
- Across the life course: for example, within the competence framework there are several areas of skills and knowledge for social prescribing practitioners related to working with children and young people, and the planned national specification will set out the expectation for services which embed the NEST framework for children and young people.
- Welsh language: for example, the planned national specification will set out the expectation for services to provide an active Welsh offer
- Relationship focused: for example the competence framework places safe, supportive, compassionate relationships and a trauma informed approach as central to a role of a social prescribing practitioner.
A wellbeing coordinator in Rhondda Cynon Taf said:
Sometimes it is just information, advice, and guidance…sometimes it’s just being with an older person who’s a bit lonely and they’re looking for local groups in their community…sometimes it is very soft support: they come and go, and that’s it. Or it could be that someone is coming to you with so many needs that they’ve got to the point where they don’t know what to do…They come with all of these impacted needs, and then I try to make a bit of a short, medium [and] long-term plan.
A young person said:
With help from [Social Prescribing Practitioner] I was able to create a more sustainable routine which I’ve started and it’s really helped me feel more physically full of energy when I wake up every day…[I now] feel more focussed in more of my classes...Also, with my social anxiety, it pushed me to be more outgoing with extracurricular activities like part time work or work placement opportunities.
5.3 Products of the national framework for social prescribing
Shared understanding
To aid this shared understanding of social prescribing, an explainer video, glossary of terms and a suite of case studies have been developed. The glossary of terms [footnote 27] is primarily aimed at professionals, with a version for the public also published.
Alongside this, we will develop a communications programme to raise awareness amongst the public and professionals as to what social prescribing is and the benefits it can bring.
Support workforce and drive up skills
A competence framework for social prescribing practitioners in Wales creates a ‘common currency’ of core knowledge, skills and behaviours. This enables more consistency between sectors and supports the integration of services. It has been developed to identify specific and measurable capabilities in which core skills and knowledge are recognised and transferrable when people move between roles, organisations or locations.
Alongside this, we will launch a skills and knowledge programme containing a suite of training courses and resources to provide the skills, techniques and knowledge needed to help people who engage with social prescribing.
Quality of provision
We will publish guidance which sets out the national standards required of community assets to ensure quality and safety within a social prescribing context. It will set out the expectation for informal and more formal interventions and draw together information on standards already in existence. It is expected to be completed by summer 2024.
Alongside this, we will explore how we can use technology to support the delivery of social prescribing and to capture activity and outcome information.
Monitor and evaluate
We will publish guidance which sets out the core data to be collected by organisations whose primary function is to deliver social prescribing, and which will support the effective performance and evaluation of social prescribing. It is expected that this will be completed by summer 2024.
This will help inform research into the benefits of social prescribing and an evaluation of the impact of social prescribing in Wales.
Improve outcomes
We will develop a national specification for social prescribing in Wales. It will provide more detail on the model of social prescribing in Wales; set out an outcomes framework from a user, organisation, commissioner and referrer perspective; and set out the overarching principles for commissioning social prescribing.
It is expected that this will be completed by summer 2024.
5.4 Driving the implementation of the national framework for social prescribing
Our consultation exercise found a lack of clear leadership, cohesion and collaboration amongst partners in social prescribing, with more effective partnership working needed to ensure sustainability and to avoid duplication.
A Wellbeing Partnership Board chaired by the Deputy Minister for Mental health and Wellbeing has been established to deliver the remaining components of the NFfSP. However, the importance of Regional Partnership Boards (RPBs) demonstrating leadership in the implementation of the NFfSP will be a key factor in its success.
RPBs will need to ensure that social prescribing is a priority, alongside the development of community assets, and demonstrate how social prescribing has become part of the integration agenda across health and social care.
To fully embed the NFfSP across Wales, we will set out an expectation for each RPB to nominate a social prescribing champion to lead developments within their respective region, linking in closely with other partnership boards such as the Public Services Boards (PSBs) and Pan Clusters Planning Groups, and to report accordingly on how social prescribing is progressing within their region.
We will also commission an independent evaluation of the NFfSP’s impact. This will allow us to gather information, learn from experience and expand the evidence base.
A clinical lead occupational therapist, a referrer to social prescribing services, Betsi Cadwaladr University Health Board area said:
This person had lost a parent, and…they were consumed by grief… So, the practitioner did a bit of work with them, explaining how grief functions…what it feels like and that it’s normal…They referred them into Cruse…Then they said, ‘When you’re waiting for Cruse, is there anything else you’d like to talk about?’. They came and said, ‘actually, I’d really like to get a bit physically fitter’.
So, after three weeks of intervention, this person was out walking the dog again…they were out doing stuff that was important to them.
5.5 Summary of ‘we will’ statements
We will develop a communications programme to raise awareness amongst the public and professionals as to what social prescribing is and the benefits it can bring.
We will launch a skills and knowledge programme containing a suite of training courses and resources to provide the skills, techniques and knowledge needed to help people who engage with social prescribing.
We will publish guidance which sets out the national standards required of community assets to ensure quality and safety within a social prescribing context.
We will explore how we can use technology to support the delivery of social prescribing and to capture activity and outcome information.
We will publish guidance which sets out the core data to be collected by organisations whose primary function is to deliver social prescribing.
We will develop a national specification for social prescribing in Wales.
We will set out an expectation for each RPB to nominate a social prescribing champion.
We will commission an independent evaluation of the NFfSP and its impact.
Annex A: list of task and finish group members
- Aneurin Bevan University Health Board.
- Arts Council of Wales.
- Future Generations Commissioner for Wales Office.
- A general practitioner.
- Health Education and Improvement Wales.
- Mind Cymru.
- Natural Resources Wales.
- NHS England.
- Powys Association of Voluntary Organisations.
- Public Health Wales.
- Royal College of General Practitioners.
- Royal College of Occupational Therapy.
- Royal College of Psychiatrists.
- Sport Wales.
- Strategic Programme for Primary Care.
- Wales Council for Voluntary Action.
- Wales School for Social Prescribing Research.
- Well North Wales.
- Welsh Government.
- Welsh Local Government Association.
Annex B: references
[1] Elliot et al. 2022
[2] Such as how we feel about ourselves and our ability to influence things that happen to us, and emotional factors, including how we understand, regulate and express our emotions and how we recognise and react to others emotions.
[3] Rempel et al. 2017
[4] Torjesen, I (2016) Social prescribing could help alleviate pressure on GPs, British Medical Journal 352; 1436.
[5] Social prescribing: an alternative approach to reduce the reliance on the NHS and social care services in Wales | University of South Wales
[6] Polley, M.,¹ Bertotti, M.,² Kimberlee, R.,3 Pilkington, K.,4 and Refsum, C. 2017 ‘A review of the evidence assessing impact of social prescribing on healthcare demand and cost implications’. University of Westminster.
[7] Kimberlee, R., Ward, R., Jones, M, and Powel, R. (2014) Measuring the economic impact of Wellspring Healthy Living Centre's Social Prescribing Wellbeing Programme for low level mental health issues encountered by GP services Bristol: University of the West of England
[8] Longwill, A, (2014) Independent Evaluation of Hackney Well Family Service, Family Action.
[9] Kellezi, B., Wakefield, J.R.H., Stevenson, C., McNamara, N., Mair, E. , Bowe, M., , Wilson, I. and Halder, M.M. (2019) The social cure of social prescribing: a mixed-¬methods study on the benefits of social connectedness on quality and effectiveness of care provision. BMJ Open 2019;9:e033137. doi:10.1136/ bmjopen-2019-033137
[10] Dayson, C. and Bashir, N. (2014) The Social and Economic Impact of the Rotherham Social Prescribing Pilot: Main evaluation report Sheffield Hallam University Centre for Regional Economic and Social Research.
[11] Social prescribing: an alternative approach to reduce the reliance on the NHS and social care services in Wales | University of South Wales
[12] Farmer, C., Fenu, E., O’Flynn, N., Guthrie, B. (2016) Clinical assessment and management of multimorbidity: summary of NICE guidance BMJ 2016;4843(September):i4843.
[13] Chatterjee, H.J., Carnie, P.H., Latyer, D. and Thomas, L.J. (2018) Non-clinical community interventions: A systematic review of social prescribing schemes Arts and Health 10(2):97-123.
[14] Kilgarriff-Foster, A. and O’Cathain, A. (2015) Exploring the components and impact of social prescribing Journal of Public Mental Health 14(3):127-134.
[15] Woodall, J., Trigwell, J., Burgon, A-M, Raine, G., Eaton, V., Davis, J., Hancock, L., Cunningham, M. and Wilkinson, S. (2018). Understanding the effectiveness and mechanisms of a social prescribing service: A mixed methods analysis BMC Health Services Research 18:604.
[16] Foster, A., Thompson, J., Holding, E., Ariss, S., Mukuria, C., Jacques, R., Akparido, R. and Haywood, A. (2020) Impact of social prescribing to address loneliness: A mixed methods evaluation of a national social prescribing programme Health and Social Care in the Community 29(5):1439-1449.
[17] Bragg, R., Wood, C., Barton, J. and Pretty, J. (2015) Wellbeing Benefits from Natural Environments Rich in Wildlife University of Essex: Colchester.
[18] Twotig-Bennett, C. and Jones, A. (2018) The health benefits of the great outdoors: A systematic review and meta-analysis of greenspace exposure and health outcomes Environmental Research 166:628-637.
[19] Leavell, M.A., Leiferman, J.A., Gascon, M., Braddick, F., Gonzalez, J.C. and Litt, J.S. (2019) Nature-based social prescribing in urban settings to improve social connectedness and mental wellbeing: A review Current Environmental Health Reports 6;297-308.
[20] Hartig, T., Mitchell, R., De Vries, S. and Frumkin, H. (2015) Nature and health Annual Review of Public Health 35:207-228.
[21] Fancourt D, Aughterson H, Finn S, Walker E, Steptoe A. How leisure activities affect health: a narrative review and multi-level theoretical framework of mechanisms of action. Lancet Psychiatry. 2021 Apr;8(4):329-339. doi: 10.1016/S2215-0366(20)30384-9. Epub 2021 Feb 11. Erratum in: Lancet Psychiatry. 2021 Feb 23;: PMID: 33581775; PMCID: PMC7613155.
[22] Right to play, Play Wales
[23] Making every contact count, Public Health Wales (nhs.wales)
[24] About us | Help me quit
[25] These findings are presented whilst also acknowledging there are limitations when using an online survey to gather data.
[26] Social Prescribing Interfaces
[27] 'Speaking the same language: A scoping review to identify the terminology associated with social prescribing'. Newstead, Eliott, Cavanagh, Tetlow and Wallace (2023) Primary Health Care Research and Development
