The role of outpatients in transforming planned care in Wales
A three-year strategy and action plan 2023 to 2026: August 2023.
A PDF download of this document will be available soon.
In this page
Foreword
In our Strategy transforming the way we deliver outpatients in Wales: A three-year strategy and action plan 2020 to 2023 NHS Wales and the Welsh Government recognised the need to modernise outpatients, ensuring the best possible care for patients.
- To deliver improved and more efficient services for patients - with the specialist medical advice and access to the right information.
- To enable patients to be seen in the right place, at the right time, and by the most appropriate healthcare professional.
- To ensure that every interaction adds value and understanding for both the patient and the clinician.
Even though some good progress was made, the onset of the coronavirus pandemic had a significant impact on planned care service delivery. Some services were paused to enable NHS organisations to respond to the immediate demands and challenges of the pandemic. As a result, waiting lists have grown, and are likely to continue growing over the coming months as people who deferred being seen during the height of the pandemic come forward to be seen, diagnosed, and treated. This has resulted in more people waiting longer than ever before for treatment and follow-up reviews.
Our programme for transforming and modernising planned care and reducing waiting lists in Wales announced by the Minister for Health and Social Care in Wales in April 2022 sets out a number of clear priorities for action up to 2026 and this strategy has been developed to deliver on those priorities through transformation of planned care services in line with A Healthier Wales. This strategy is committed to helping people in Wales to access health advice and the services they need, when they need it as set out in the Recovery Plan:
- we will increase health service capacity
- we will prioritise your diagnosis and treatment
- we will transform the way we provide planned care
- we will provide better information and support to patients
This strategy and action plan sets out our intentions to recover, reset and transform planned care services whilst reducing variation across health boards and deliver consistent and equitable services for all. It has been developed to support clinical teams within the NHS in Wales to deliver sustainable, modernised, responsive, and equitable outpatient services as part of planned care to the people of Wales.
- Focusing on clearing the backlog of those waiting for treatment by creating additional activity.
- Resetting the service with a focus on a value-led and efficient service model.
- Driving transformation by embedding sustainable change.
Introduction and background
Even before the pandemic waiting times and delays in accessing care were increasing, clearly showing the unsustainability and fragility of the traditional planned care model. The coronavirus pandemic exacerbated this position with the need to periodically suspend planned care to deploy resources to respond to the challenges of the pandemic resulting in more people waiting longer for care than ever before.
Our programme for transforming and modernising planned care and reducing waiting lists in Wales, announced by the Minister for Health & Social Care in April 2022, clearly sets out our ambitions to improve the way planned care will be delivered in the future. This will require new solutions and the need to embed new ways of working, ensuring there is wellbeing support for those who are waiting whilst building sustainability and resilience into the system.
Following publication of the 'outpatients strategy' in 2020, the evidence showed that prior to the onset of COVID, progress was being made to transform. The implementation of alternative person-centred approaches resulted in the follow-up reduction targets being met, releasing capacity to see those who needed to be seen sooner.
During COVID, health boards demonstrated their ability to increase the pace in implementing these new ways of working. Supported by implementation toolkits and a national website, progress was made in delivering virtual appointments and reviews, and supported self-management models. Despite this, care continues to remain largely based on visits to hospitals. We need to accelerate this shift to develop value-based, tailored patient care aimed at minimising disruption to patients’ and carers’ lives, improving the patient experience and ensuring that the majority of care is provided closer to home.
Despite the challenges presented by COVID, at the height of the pandemic, up to 54% of hospital appointments and reviews were being undertaken virtually to provide continuity of care across Wales. The video group clinic model was also developed.
We now need to sustain and further accelerate the rate of this change and develop more person-centred services that empower people to self-manage their condition better in partnership with clinical services. We need to better communicate with patients and public, providing evidence-based advice, guidance, and support to make healthy lifestyle choices, prevent deterioration and be better prepared for treatment and recovery. And we need to do this in collaboration with other policy areas to ensure strategic alignment that supports more integrated and seamless care.
Through this strategy, and the health transformation boards, we will ensure that services continue to transform in line with the priorities set out by the Minister and move forward together to address the backlog by transforming outpatients to deliver quality, person-centred planned care services to the people of Wales.
Our vision
To enable people to receive the right care, right information, from the right person, at the right time, in the right place, so they can maximise their health and well-being status and stay independent as long as possible.
We will support this by ensuring that people get fast access to advice information and support, developing self-management systems, virtual reviews and, where needed, get timely access to the appropriate health care professional as close to home as possible.
Patient engagement – what did we learn
People have told us what can go wrong for them when they have been referred to outpatients:
- the length of wait to get an appointment to see a consultant
- not knowing how long they will have to wait to get an appointment to see a consultant
- no support or advice whilst waiting to be seen/treated
- cancellation or rearrangement of appointments – sometimes at the last minute
- often unable to park or find their way around the hospital
- the treatment process or their pathway is not explained very well
- not knowing what to expect from an appointment – or why they are there
- no clear guidance on what to do in an emergency
- having to constantly repeat / provide personal and clinical details
- poor communication and explanations
- feeling under pressure to say ‘no’ when they are contacted to ask if they want to remain on a waiting list
- not realising they are on a waiting list
- confusion when on multiple waiting lists and pathways
Where are we now and what does the data tells us
Chart 1: Annual referrals from the period between 2018 and 2023

Referrals
- In 2018/19 (pre-COVID) there were 1.35 million referrals from primary care (e.g., GPs, optometrists) for a new outpatient appointment.
- In 2022/23 the number of referrals increased by 5% to 1.42 million.
- 134,150 referrals were made into specialist care in March 2023 – an average of 4,328 per working day.
This is the highest ever rate recorded in Wales.
Open RTT pathways
- In March 2022, the number of people in Wales on an open RTT pathway was 701,411.
- In March 2023, this had increased by 4.75% to 734,721.
Chart 2: Numbers waiting on an open RTT pathway in the planned care specialties: March 2023
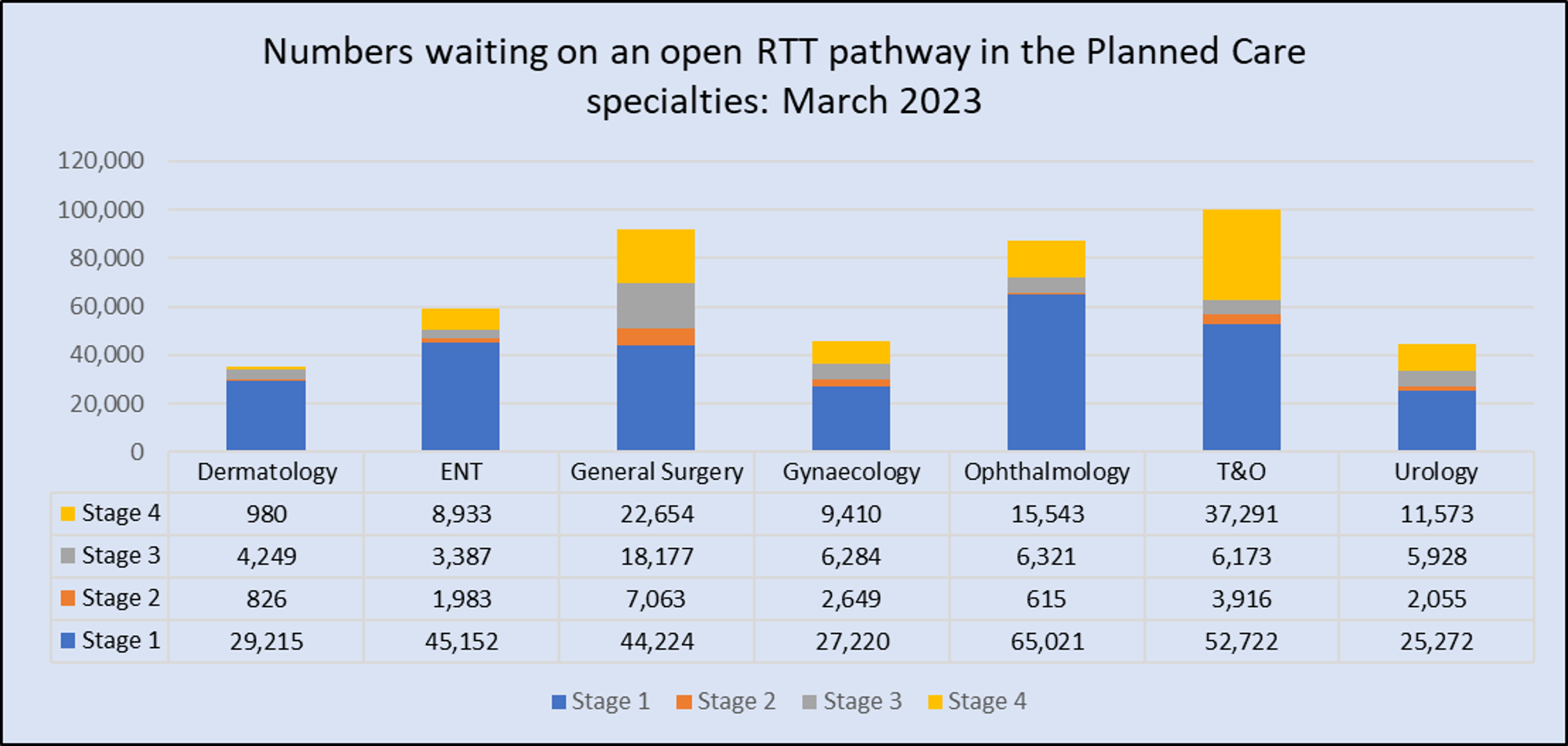
New outpatients
- In March 2022, the number waiting over 52 weeks for a first appointment in the 7 planned care clinical specialties was 76,396.
- In March 2023, this number had reduced by 40% to 45,792.
| Department | March 2022 | March 2023 |
|
Ophthalmology |
16,911 | 14,021 |
| Ear, Nose and Throat | 15,481 | 10,145 |
| Orthopaedics | 15,802 | 7,130 |
| General Surgery | 11,441 | 4,271 |
| Urology | 8,567 | 5,789 |
| Dermatology | 5,026 | 4,090 |
| Gynaecology | 3,168 | 346 |
Promote, Prevent and Prepare for planned care
The 3Ps policy
This policy ensures that support and information is easily accessible to those referred into specialist planned care services. We must ‘change the narrative’ to move away from the passive waiting list to pro-active waiting by empowering people to better self-manage their condition, make healthy choices, prevent deconditioning and prepare for positive outcomes for their treatment and recovery.
Follow ups
790,628 people were on a follow-up waiting list in March 2022.
By March 2023, this number had increased by 14.7% to 906,669.
Chart 3: Total number FUWL per health board
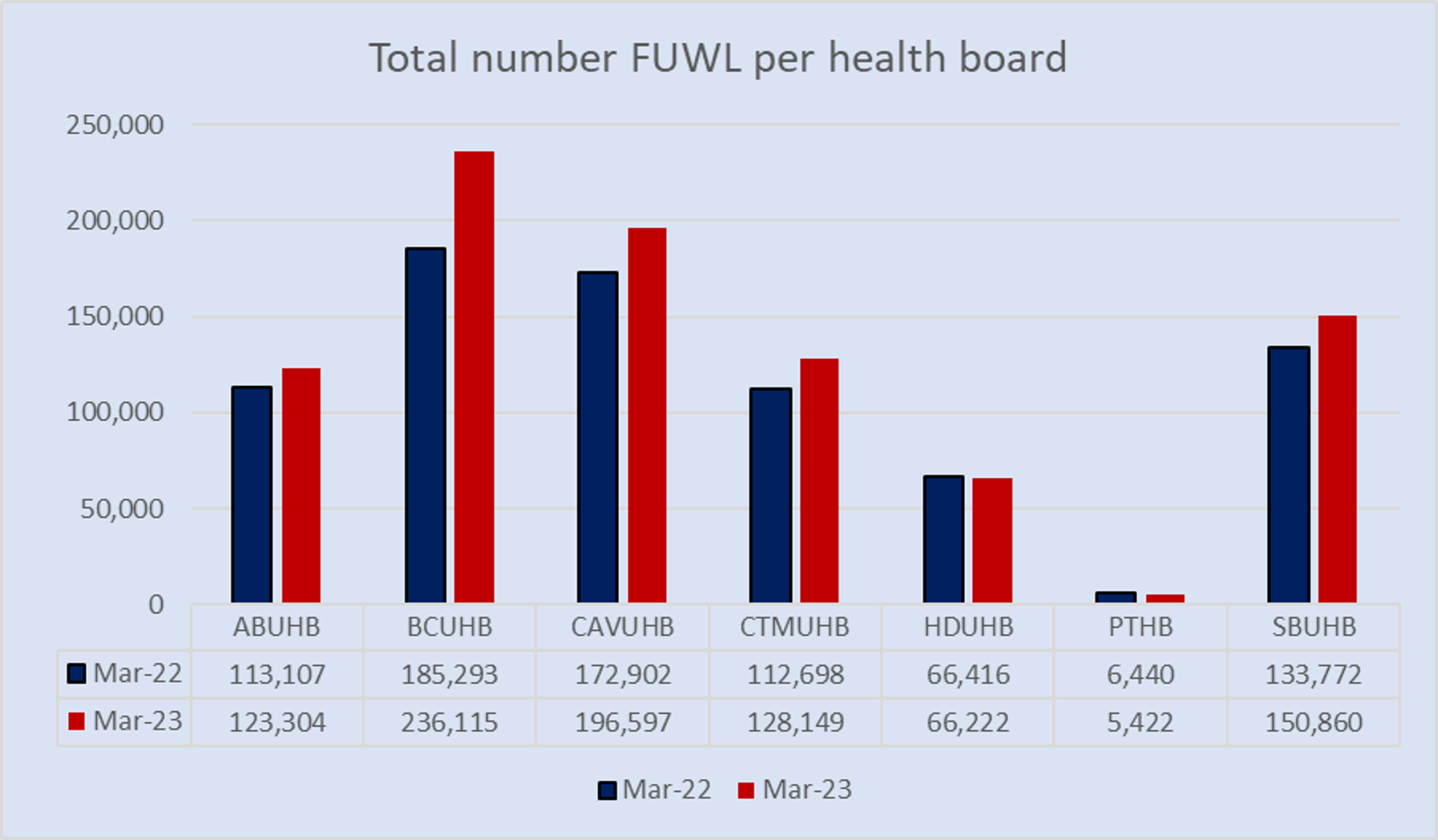
The total follow-up waiting list has increased in all planned care clinical specialties.
Chart 4: All Wales FUWL for planned care specialties

Over 100% delayed
- In March 2022, 195,986 people were delayed over 100% past their follow-up target date.
- By March 2023, this number had increased by 25.9% to 246,662.
- Over 27% of the people on the total follow-up waiting list were over 100% delayed past their target date in March 2023.
Chart 5: Over 100% follow up for planned care specialties.

- Referrals have recovered to, and exceeded, pre-COVID levels. However, the capacity to deliver has not, leading to unprecedented backlogs.
- Waiting lists continue to grow.
- The number of people on a follow-up waiting list is growing.
If we do not transform the way we deliver services, the backlog will continue to grow. Alternatives to routine follow-ups need to be maximised. Not only will this ensure value-based health care, but it will also release capacity to see those who need to be seen sooner.
A new approach: What needs to change
Change is happening in NHS Wales, but we need to accelerate the pace of change to recover and transform. We need to continue to take a more coherent and collaborative approach to achieve sustainable change.
- An outpatient appointment, including routine follow-up, should not be the automatic default for the delivery of care.
- An outpatient appointment should have a clear purpose to diagnose or provide treatment options for a patient.
- Conveying information on regular test results, reviewing a pathway or discharge does not always need to happen face-to-face, or on a one-to-one basis.
- All interactions should be value-based.
- Multi-disciplinary skills and capacity needs to be fully utilised.
Referrals in the future
There is good evidence that change is happening in our hospitals. We need to sustain and accelerate this change.
An appointment should not automatically be offered. The clinician may:
- provide advice regarding the treatment plan via the integrated e-referral platform
- send straight to test to avoid delays in the patient pathway
- send directly to pre-assessment for treatment
- allocate to a member of the multi-disciplinary team, for example, specialist nurse, allied health professional
- send to another service if appropriate
- accept the referral and prioritise based on clinical need
On-going care in the future
Before a follow-up appointment is offered, consider:
- Will the appointment ‘add value’ to the patient’s care?
- Is there a better alternative to a face-to-face appointment?
- Who is best for the patient to talk to/see?
Think about:
- discharge back to primary care with a management plan
- discharge with an option to be reviewed based on supported self-management if there is a change in their symptoms such as SOS, PIFU or self-management platforms)
- review supported by a patient reported outcome measurement or PROMS.
- virtual reviews including attend anywhere video or telephone or via a desk top review.
- multidisciplinary review and joint clinic
- peer support through expert patient programmes. Group clinics and video group clinics.
The policy context and strategic framework
The diagram below illustrates the strategies and programmes which inform, underpin, compliment and are aligned with the outpatient strategy in terms of whole system change.
The meta-policy: A Healthier Wales
The Recovery Plan: Our programme for transforming and modernising planned care and reducing waiting lists in Wales
Who will deliver:
- Welsh Government
- NHS Executive
- NHS Wales
- Strategic programme for planned care
- Outpatients transformation programme
- Health and care pathways programme
Strategies
- 5 Goals for planned care
- outpatients transformation strategy
- Diagnostics strategy
- Cancer strategy
Underpinning principles/influencing factors
- Prudent healthcare
- Allied health professionals framework
- Value in health
- Making every contact count
- Digital services for patients and public programme
- NHS quadruple aim
- Welsh language measures
- Wales Audit office - Management of follow up out-patients across Wales
- The Wellbeing of Future Generations Act (2015)
- GIRFT review
- Further, Faster
Aligned with
- National clinical framework
- Strategic programme for primary care
- 6 Goals for urgent and emergency care
The planned care 5 goals strategy
Published in September 2021, the 5 goals for planned care provides a strategic vision for the future of planned care services in Wales. It aims to address the two related challenges currently faced:
- to support recovery following the coronavirus pandemic
- to develop sustainable NHS services that are able to respond to the year-on-year increase demand for planned care services across Wales.
Together with the priorities identified within the National Clinical Framework, the NHS Planning Framework and the vision set out in A Healthier Wales, the five goals for planned care underpin the Recovery and Transformation Plan announced by the Minister in April 2022 to ensure the development and provision of sustainable, prudent, and value-based services as close to home as possible.
NHS Wales and the Welsh Government will continue to support the implementation of new, innovative, and ambitious approaches to service transformation.
Goal 1: Effective referral
Ensure that referral guidance and thresholds are in place to ensure that those most in clinical need are referred to the appropriate setting.
Goal 2: Advice and guidance
Develop access to high quality advice and guidance to enable informed decision making for individuals as well as primary and secondary care clinicians.
Goal 3: Treat accordingly
Access to the appropriate care at the right time at the right place.
Goal 4: Follow up prudently
Giving individuals more choice and control over their care.
Goal 5: Measure what’s important
Transforming care to better meet the clinical needs of the patient.
Delivering the 5 goals strategy
Goal 1: effective referral
Ensure that referral guidance and thresholds are in place to ensure those most in clinical need are referred to the appropriate setting.
Enablers
The health and care pathways programme:
- digital pathways platform
- referral guidance
- do not do/interventions not normally undertaken policy
- alternative pathways
- patient support and information
- integrated e-referral and e-advice
Goal: 2. advice and guidance
Develop access to high quality advice and guidance to enable informed decision making for individuals as well as primary and secondary care clinicians.
Enablers
The Health and Care Pathways Programme:
- remote advice and guidance
- integrated e-referral and e-advice
- remote triage
- straight to test
- advice, guidance, and support to empower patients to better self-manage their condition and prepare for treatment and recovery
Goal 3: treat accordingly
Access to appropriate care at the right time at the right place.
Enablers
- artificial intelligence
- diagnostic and treatment centres
- regional specialist centres and other regional solutions
- efficient use of resources
- patient support and communication
- 3Ps services
Goal 4: follow up prudently
Giving individuals more choice and control over their care.
Enablers
- 'discharge as default’
- see on symptoms and patient initiated follow up – including digital approaches
- supported self-management pathways – including digital approaches
- virtual reviews – synchronous and asynchronous
- patient reported outcome measures
- follow up guidance
Goal 5: measure what’s important
Transforming care to better meet the clinical need of the patient.
Enablers
- modernised outpatient dataset
- effective demand and capacity planning
- validation
- local and national dashboards
- new approach to referral to treatment incorporating new ways of delivering services
- embedding 'patient reported outcome measures' and 'patient reported experience measures' into pathways
Challenges
Patients and public
- population health
- rurality/geography/boundaries
- not attending appointments – not seeing value in attending appointments
- not understanding how the health system works
- delays in receiving care and associated risk of deconditioning, clinical harm and impact on wellbeing and wider needs
- feel unsupported along their health care journey
- not involved in decision making regarding their own care and system design
System pressures
- environmental and estate limitations
- booking processes
- conflicting priorities
- inefficiency of the current system – HIC, DNA (hospital initiated cancellations, did not attend)
- data quality
- need to accelerate pace of change
Workforce
- leadership to drive change
- clinical engagement to work differently
- scale of whole system transformation
- time to dedicate to making changes
- recruitment and retention challenges
- inflexible job-planning
Demand for services
- demand/capacity imbalance
- increased delays in providing care
- activity/service delivery
- COVID backlogs
- increased number of people being referred
- increased delays in care
- increasing reliance on waiting list initiatives and extra sessions
What we want to achieve
Prudent healthcare
- people are seen in the right place, by the right person at the right time
- only those who need specialist care are seen in secondary care
Person-centred care and co-production
- care and treatment is planned based on individual needs
- people are treated holistically, supporting health and well-being at all stages of their care pathway, including healthier lifestyle choices, support whilst waiting and preparation for treatment and recovery
- people are empowered to be in control of their health journey and make decisions about their treatment and ongoing needs
- delivery of integrated care
Value in health
- measuring value for money and benefits of social investment
- all care is underpinned by value in health principles
- develop systems that enable effective service delivery planning including demand and capacity
- measure the impact of services on people’s health and well-being
- reduce unwanted variation
Once for Wales
- develop standardised national models and resources which can be localised and adopted across Wales
- maximise spread and scale opportunities
- create a culture of innovation and adopting best practice
Evidence based care and ‘best in class’
- people have access to care, which is based on best clinical evidence, value-based, and available to everyone wherever they live in Wales
- comparing services in Wales with world leading providers to learn what we can do better
- GIRFT reviews
Digitalisation
- developing systems in partnership with patients to provide access to information about their care pathway, education tools, decision-making aids, and patient-facing platforms
- working in collaboration with other policy areas in the development of digital applications
Goal 1: effective referral
Deliverable: Health and care pathways programme
Health boards and trusts will deliver the outcomes identified within the health and care pathways programme including:
- digital pathways
- remote advice and guidance
- integrated e-advice and e-referral
Progress
- programme funded by the planned care recovery fund. Commitment made for 2023 to 2026
- programme team in place
- the National Pathways Implementation Group (NPIG) arrangements are now in place, with assistance of the NHS Exec programme team, pathway alliance team and programme leads from each health board.
- the health and care pathways Cymru operational group set up to ensure alignment with health board plans
Action required
Memorandum of understanding to be finalised by NWSSPs commercial team for health board sign-off.
Deliverable: digital pathways
- platform procured – pathways alliance
- pathway alliance training for health boards commenced
- health board clinical editors being recruited
Progress
- the programme to be implemented sequentially by individual health boards
- training programme for clinical editors
- develop platform
- confirm initial 21 pathways for development
- develop nationally agreed pathways
- localise nationally agreed pathways
Delivery
2023 to 2026
Goal 2: advice and guidance
Deliverable: health and care pathways programme
Health boards and trusts will deliver the outcomes identified within the Health & Care Pathways Programme including:
- remote advice and guidance
- integrated e-advice and e-referral
Progress: Remote advice and guidance
Remote advice and guidance:
- consultant Connect procured to deliver
- the national remote, advice and guidance group arrangements
- ‘Gap analysis’ produced of sub-specialities by individual health board to support to roll out
Action required
- all health boards and consultant connect to deliver on key deliverables as set out in the project initiation document
- formalise reporting arrangements in line with identified KPIs.
Delivery
2023 to 2026
Progress: integrated e-referral and e-advice
- implemented in 6 health boards
- pilot shows 15% activity returned as advice only
Action required
- to complete roll-out in all health boards and trusts
- to formalise reporting arrangements in line with identified KPIs
Delivery
March 2024
Deliverable: the 3Ps policy
Development and implementation of the 3Ps policy and self-assessment tool for services to support people to maximise health and well-being:
- Promote healthy lifestyles and improved health behaviours
- Prevent deconditioning and worsening health
- Prepare for treatment, recovery, and on-going good health
Phase 1: Those already on a waiting list/pathway and their families and carers.
Phase 2: New people being referred to specialist services and their families and carers.
Progress
- steering group and development group in place to lead on this work
- 3Ps policy and self-assessment tool under development
Action required
- publish ministerially approved 3Ps policy and self-assessment tool by July 2023
- all health boards to deliver on outcomes identified within Phase 1 of the 3Ps Policy delivery plan and service specification (March 2024)
- all health boards to deliver on outcomes identified within Phase 2 of the 3Ps Policy delivery plan and service specification (March 2025)
- all health boards to implement and embed as business as usual the virtual joint school model to help people prepare for surgery – model and toolkit developed (March 2024)
- link with Planned Care information campaign to support communication and engagement with the public (September 2023)
- link with CAVUHB regarding roll out of a public facing ‘Keeping Me Well’ website (March 2024)
Deliverable: Improve communication with the population regarding health board waiting times
- Phase 1: access to information on waiting times
- Phase 2: signposting to support and information to support people in line with the 3Ps policy
Progress
Access to waiting times information (by health board and by specialty) launched on the NHS 111 website in November 2022 (Phase 1). This work is being led by WG.
Action required
Refine information provided following feedback from the public for launch in Phase 2 (July 2023).
Progress
Include signposting to information and services available to support people preparing for treatment on NHS Wales 111 site. (Phase 2).
Action required
- national resources identified and website pages in process of being developed – this work is being led by WG (July 2023)
- all health boards to ensure they have processes in place to signpost patients to the information on the NHS Wales 111 website supported by local waiting list information for specific conditions, for example, hip arthroplasty, knew arthroplasty (December 2023).
Deliverable: planned care public information campaign
- develop a suite of social media resources to raise awareness of new ways of accessing services moving forward
- raise awareness of ‘Waiting Well’ and 3Ps.
Progress
- WG led
- working in collaboration with the WG communications team to develop social media assets for health boards
Action required
- finalise planned care public information campaign assets (July 2023)
- liaise with health board communications teams to include resources developed on local websites (December 2023).
Goal 3: treat accordingly
Deliverable
Health boards to maximise the use of community and one-stop clinics.
Progress
Progress remains varied across Wales. There are some examples of good practice which have been developed and shared and have potential for local adoption.
Action required
- to embed as business as usual across Wales to provide a consistent and equitable national offer
- explore toathway redesign to maximise resources across the health care system and deliver integrated care.
Delivery
2023 – 2026
Deliverable
Clinician should consider the most appropriate mode of appointment for the patient, providing flexibility and choice: face-to-face or virtual; synchronous (direct patient contact) or asynchronous (indirect patient contact); one-to-one or group appointment, whilst maximising the skills and capacity within the multi-disciplinary team.
Progress: virtual approaches
- virtual appointments implemented at pace during covid: up to 54% appointments delivered virtually
- Data Standard Change Notification (DCSN) approved and systems updated to record and report virtual activity
- implementation toolkit developed
Action required
- maximise the use of virtual approaches in outpatient delivery for both new and follow-up appointments
- public-facing information regarding all virtual approaches to be communicated via health board websites
Delivery
2023 to 2026
Progress: video group clinics
- video group clinic model developed, and training provided to teams
- best practice toolkits developed
- Data Standards Change Notice (DSCN) and interim reporting arrangements developed (to be incorporated in modernised outpatient dataset development as sustainable solution)
- all relevant governance arrangement in place
- formal evaluation undertaken
Action required
- maximise use of allied health professional and specialist nurse capacity to deliver clinics to release consultant capacity to see those with more complex needs (2023 to 2026).
- minimum of 10 new video group clinic/face-to-face group clinic models to be implemented in each health board (March 2024)
- minimum of 10 additional video group clinic/face-to-face group clinic models to be implemented in each health board (March 2025)
- minimum of 10 additional video group clinic/face-to-face group clinic models to be implemented in each health board (March 2026)
Deliverable: Implement an all-Wales teledermoscopy service that enables remote reporting of skin lesions images
- enabling patients with skin lesions to receive their diagnosis in a timelier manner
- releasing capacity in dermatology clinics enabling those patients with the greatest clinical need to be seen face to face
- address the dermatology waiting list backlog
Progress
- teledermoscopy pathway endorsed by the Dermatology Clinical Implementation Network
- services established in 4/6 Health Boards that deliver dermatology care
- development of standardised cross boundary recharge process to facilitate cross boundary reporting
Action required
- electronic referral system to be activated within all health boards to facilitate timely referrals across dermatology and medical illustration
- service establishment across remaining health boards
- national evaluation of all Wales service to demonstrate impact
- integration of medical imaging management systems with Welsh clinical portal
- explore how the model can be adapted for other pathways, for example, tele-ear throat and nose, Tele-MaxFax
Delivery
March 2024
Deliverable
Development of an evidence-based interventions not normally undertaken (INNUs) policy in Wales to ensure consistency and address health inequalities.
Progress
- Health Technology Wales (HTW) and the Welsh Value in Health Centre (WVHC) to collaborate to update the evidence base of INNUs
- common list of 15 INNUs agreed
Action required
- to complete pilot
- to undertake evaluation
- to implement nationally
Delivery
March 2024
Goal 4: follow up prudently
Follow-up and on-going care are based on agreed clinically agreed intervals supported by clinical evidence pathways. Discharge should be considered as a default, but when this is not clinically appropriate, alternatives to the traditional routine FU cycle should be considered. Alternatives to low-value routine follow-ups to be implemented at pace to deliver person-centred care that adds value to the patient’s pathway and maximises use of capacity.
Deliverable
Maximise the use of supported self-management models where clinically appropriate to deliver person-centred care underpinned by value in health principles and maximise capacity to deliver:
- see-on-symptom (SOS)
- patient-initiated follow-up (PIFU) where clinically appropriate
- eSOS platform
- Prostatic Specific Antigen (PSA) platform
Progress
- DSCN published and systems updated to record and report activity
- implementation toolkit developed
- SOS/PIFU website launched July 2022 providing professionals with toolkits, clinically approved pathways, resources, community of practice
- local dashboards developed to monitor utilisation
Action required
- all health board to increase pace of spread and scale maximising the utilisation of the website
- all health boards to increase spread and scale of the pathways developed and shared on the website
- all health boards to demonstrate an annual increase in the use of SOS and PIFU
- all health boards to include public-facing information on SOS and PIFU to that patients can maximise the benefits of being on an SOS/PIFU pathway
- consider national dashboard to support benchmarking
Delivery
2023 to 2026
Progress: eSOS platform
- development of the eSOS platform is progressing
- positive feedback from patients involved in testing the platform
- positive feedback from clinicians
Action required
- final testing (August 2023)
- formal evaluation to be undertaken to consider next steps (March 2024)
Best practice: SOS and PIFU information: Betsi Cadwaladr University Health Board
Webpages developed to provide the public with information and short animations on the benefits of the pathways and how to self-manage their condition better when on the pathways.
Deliverable: PSA platform
Implement an all-Wales digital platform to provide a model of care which empowers individuals living with prostate cancer to manage their own health condition remotely. In turn releasing capacity within Urology services to provide those who need outpatient care to receive timely access.
Progress
- my medical record (MyMR) platform procured as an all-Wales platform
- implementation and integration commenced in health boards
- patient supporting documentation produced, including creation of web-page
Action required
- local integration development
- national Integration feeds via DHCW to facilitate national roll out
- agreement of ongoing support and governance system following programme closure
Delivery
March 2024
Goal 5: measure what’s important
Deliverable
Develop a national and sustainable approach to waiting list validation and 6 monthly ‘keeping in touch’ process for those waiting over 52 weeks and embed as business as usual linked to the 3Ps policy area.
Progress
- wide variation across health boards
- validation processes undertaken intermittently
Action required
- all health boards to embed an agreed standardised on-going validation process into business as usual
- all health boards to embed 6 monthly check-ins with those waiting over 52 weeks linked to local 3Ps services.
Delivery
March 2024
Deliverable
Develop a modernised outpatient dataset (MODS) to provide quality data that reflects the modernised outpatient service delivery model. New MODS will contribute to more effective demand and capacity and service delivery planning.
Work led by DHCW in partnership with Planned Care Programme leads (WG and NHS Executive) and health boards.
Progress
- MODS steering group set up
- some challenges which have impeded pace of progress - issues being addressed
- project plan in place
Action required
- define modernised dataset to reflect new service delivery model
- publish Data Standard Change Notice
- update patient administration systems to support changes
Delivery
March 2026
Deliverable
Embed patient reported outcome measures (PROMS) and patient reported experience outcomes (PREMS).
Progress
Further development work required to develop a nationally agreed and standardised process.
Action required
- to work with partners in Value in Health to develop a standardised approach and supporting resources (December 2023)
- all health boards to embed into clinical pathways to support patients preparing for treatment (3Ps policy) (March 2025)
- all health boards to embed into clinical pathways to deliver effective, person-centred on-going care (March 2025)
- all health boards to embed into clinical pathways to deliver effective, person-centred on-going care (March 2025).
Delivering the strategy: Once for Wales approaches
Deliverable
Digital to become the default channel for appointments with patients including:
- notification and confirmation
- reminders
- information relating to appointments including links to support on health board website
To be developed in partnership with the Digital Services for Patients and Public (DSPP) programme as element of the NHS Wales App work.
Progress
Some health boards have implemented booking confirmation and reminders which include information regarding appointment and links to other information
Action required
- to actively promote the shift to digital channels while retaining paper-based channels for those who prefer not to use digital
- alignment to equality legislation
- all health boards to implement digital channels for information relating to appointments
- demonstrate co-production with the public
Delivery
March 2024
Deliverable
Widespread third-party open access to appointment booking systems to be developed in line with the Digital Services for Patients and Public programme as element of the NHS Wales App work.
Progress
To be commenced.
Action required
- develop common standards and open architecture approach in collaboration with the DSPP programme
- health boards and trusts to actively promote open access to appointments systems
- develop a common All-Wales information governance and access framework
Delivery
March 2026.
Delivering the strategy: summary of targets
Targets relating to new patients
No patients waiting over 52 weeks for a new outpatient appointment by December 2022.
No patients waiting over 156 weeks for a new outpatient appointment by September 2023.
No patients waiting over 156 weeks for a new outpatient appointment by 2026.
95% of patients waiting less than 26 weeks for treatment on an RTT pathway by 2026.
All patients who have waited more than 3 years for an outpatient appointment to have a booked appointment by August 2023.
97% of patients on an RTT open pathway to complete their treatment within 104 weeks by December 2023.
99% of patients on an open RTT pathway to complete their treatment within 104 weeks by March 2024.
No patients waiting over 8 weeks for a diagnostic by March 2024.
Targets relating to FU patients
To reduce the number of patients on a FU waiting list by 30% on the March 2019 baseline by March 2024.
To reduce the number of patients who are more than 100% delayed their FU appointment by 30% on the March 2019 baseline by March 2024.
SOS and PIFU activity to demonstrate an annual increase as agreed within the Outpatients Steering Group (annual).
Service delivery targets
Health boards to show an annual increase in the number of pathways where virtual appointments and reviews carried out virtually (synchronous and asynchronous) as agreed within the Outpatients Steering Group supported by the Clinical Implementation Networks (annual).
Health boards to deliver a 50% reduction in Hospital-initiated cancellations (HICs) on the March 2019 baseline (2026).
Health boards to demonstrate an annual incremental improvement trajectory to achieve the 50% reduction in HICs by 2026 (annual).
Health board DNA rate to be no more that 5% for news and follow-ups (2026).
