Technical Advisory Cell: summary of advice 23 July 2021
Summary of COVID-19 advice provided to Welsh Ministers on 23 July 2021.
This file may not be fully accessible.
In this page
Top line summary
Overall transmission of COVID-19 continues to increase in many areas across Wales, although several areas are now reducing or close to stable in terms of weekly change.
Estimates of R and the growth rate are now provided by the UK Health Security Agency (UKHSA) rather than SAGE. The UKHSA consensus estimate of the reproduction number for Wales is between 1.2 and 1.4 and a doubling time of 11 to 19 days while PHW's estimate is between 1.3 and 1.4 and a doubling time of between 10 and 23 days. Note that UKHSA’s estimate is typically lagged by 2-3 weeks while PHW, which uses a different methodology, is lagged by around 1 week.
Surveillance data continues to suggest that the link between cases, hospitalisation and deaths has been weakened by the vaccination programme.
However, COVID-19 ICU admissions have increased from a low level in the last two weeks and are now above the estimates suggested by TAC’s most likely scenario, although they remain below the reasonable worst case scenario.
Updated modelling from Swansea University comparing a scenario in which population behaviours such as social distancing are retained after 7 August and another in which behaviour fully returns to pre-pandemic norms suggests that these measures will continue to be important through the summer in order to avoid a subsequent resurgence of COVID-19.
A rapid review of the impact on the pandemic on the mental health of health and social care workers during this period suggests there was a substantial adverse impact during this time. Among the studies several common risk factors such as female staff members, pre-existing or prior mental health disorders and concerns around transmission and availability of PPE were identified, supporting the need for prioritisation and distribution of mental health support.
In a recent report by the ONS on Long COVID 3.6% of adults said they had experienced long COVID, in addition to 2.6% who said there were unsure. Of this 57% stated long-COVID had negatively affected their general wellbeing and 30% reported it had negatively affected their work.
The newest PHE Variant Technical Briefing provides updated risk assessments for the delta and beta variants. The risk of reinfection for Delta has been upgraded to a red RAG rating, although this is with low confidence due to small numbers. Currently the vast majority (86%) of Delta cases in England is in people with both no previous infection or who have not been fully vaccinated.
The AMS report on preparing for winter has been published, exploring the health and social care challenges presented by winter 2021/22. The report emphasises the need to maximise the speed and uptake of vaccination in all eligible age groups, including possible booster vaccines for COVID-19 and influenza later in the year. The paper also highlights the wider health and wellbeing impacts of the pandemic and the high likelihood that other diseases are likely to be exacerbated over the winter period.
The Royal academy of engineering has also prepared a report following a commission from SAGE, setting out the need to monitor and improve the ventilation in public buildings, as well as improving industry knowledge and skills to reduce the impact of COVID-19 and other public health issues.
Insights from SAGE 94, 22 July
SPI-M have outlined several areas of concern over the coming months, including pressure on the NHS resulting in the need to reinstate some restrictions, changes in population behaviours such as social-distancing and isolation or testing take-up and the increased transmission of other respiratory diseases such as Respiratory Syncytial Virus (RSV) or novel variants of concern.
A paper on long COVID highlights several consistent risk factors including increasing age, female sex, obesity or poor pre-pandemic fitness, pre-existing asthma and hospitalisation from COVID. Data is limited for children but suggests that long illness duration is uncommon, with around 2% experiencing symptoms 8 weeks after infection (low confidence)
It is highly likely that vaccine induced immunity to SARS-CoV-2 infection (high confidence), and potentially severe disease (but probably to a lesser extent) will wane over time (medium confidence). This is likely to be first detected by vaccine failures in vulnerable cohorts (for example a high rate of infections in people vaccinated over time, including hospitalized cases). There is no evidence of an effect of age on the peak or length of antibody responses, although prior infection was strongly associated with a higher peak level and longer half-life.
Higher transmission and circulation of SARS-Cov-2 will result in a higher risk of novel variants of concern (high confidence). Reducing viral load both nationally and globally will reduce the frequency and number of new variants arising. The biggest threat to the UK’s health security and response to the SARS-CoV-2 pandemic is the emergence (and establishment within the UK) of variants that either have increased transmissibility, increased disease severity, escape prior immunity, or a combination of these characteristics (high confidence). This includes the importation of variants that emerge internationally.
Wales Sit-Rep
Read the latest COVID-19 Situational Report, containing the most recent data on epidemiological surveillance, NHS status, education and children, international travel, mobility, vaccination and immunity and forward projections.
Overall, case numbers continue to increase across the majority of Welsh Local Authorities, with case incidence at a national level increasing by 31% in the most recent week to 190.1. Case numbers may be beginning to stabilise in some areas, with several Local Authorities seeing reducing cases or close to stable changes compared to previous weeks, but this is currently uncertain.
Case numbers continue to be highest in the 10-19 and 20-29 age groups, although the extent of the difference with other age groups varies by local authority. Initial investigation suggests that these differences do not correlate with vaccination status, with the 8 LAs above the Wales average for cases per 100,000 population in 20-29 year olds ranging from 24% to 59% fully vaccinated of this age group. This would suggest case numbers are largely driven by behaviours rather than vaccination status, although further investigation is required.
SAGE’s estimate of the reproduction number (Rt), which is typically lagged by 2-3 weeks, is between 1.2 and 1.4 for Wales, while PHW’s estimate of Rt, which is less lagged, is between 1.3 and 1.4.
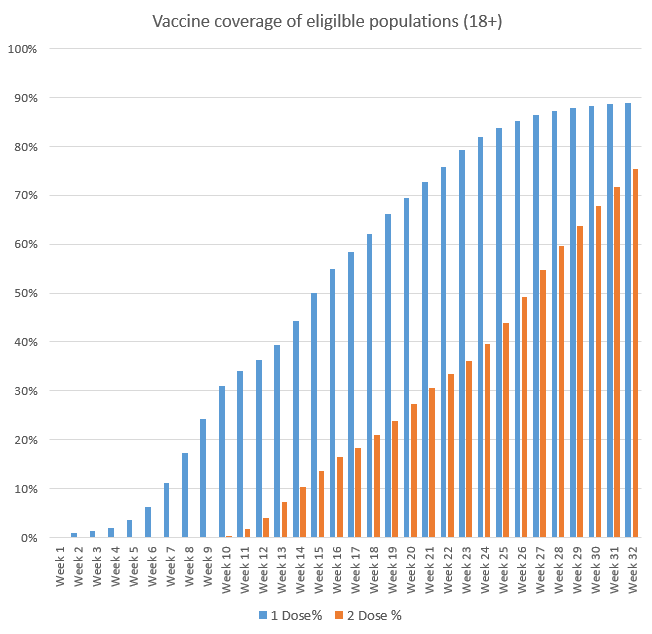
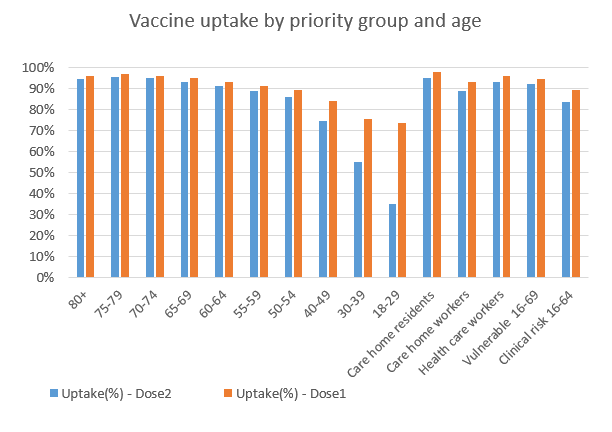
With 90% of the eligible Welsh population receiving their first dose of the vaccine, focus has largely shifted to giving people their second dose, with first dose take up for the 18-29 and 30-39 stabilising at around 75%.
Relationship between cases, hospitalisation and death
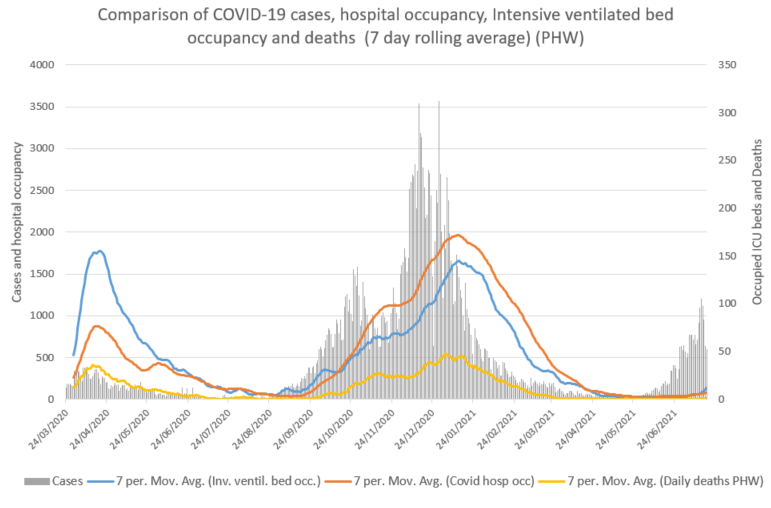
Comparison of current levels with previous waves continues to support that the link between cases, deaths and hospitalisations has been weakened by the vaccination programme, although it has not been broken entirely and these have all increased alongside cases, although to a lesser extent than previous waves.
Since the beginning of June, the 7 day average of cases have increased from 37 to 805, COVID-19 Invasive ventilated bed occupancy from 3 to 16, COVID hospital occupancy from 10 to 92 and deaths from 0 to 11 (data as at 20 July). Of the 7,813 Delta variant cases of detected as at 20 July 99, or 1.3%, have been hospitalised (Source PHW).
Reasonable worst case and most likely scenarios versus actual figures
Key message: Observed levels of COVID-19 cases, admissions to hospital, deaths and hospital bed occupancy are much lower than the levels estimated by the June 2021 reasonable worst case (RWC) scenario and are roughly at the levels estimated by the June 2021 most like scenario (MLS). COVID-19 ICU admissions have increased rapidly in the last fortnight from a low baseline to levels last seen on 20 September 2020 and are above the MLS estimates, but are below the RWC scenario estimates. COVID-19 cases have been increasing throughout June and July and hospital admissions, hospital occupancy and COVID-19-related deaths are beginning to increase, although at much reduced levels compared with previous waves.
This report compares observed levels of COVID-19 indicators with the June 2021 RWC scenario and MLS for the first time. These scenarios take account of the impact of the Delta variant.
In the charts below “RWC_Jun2021” is the June 2021 RWC scenario, “MLS_Jun2021” is the current (June 2021) most likely scenario, and “Actuals” represents the actual observed values for each indicator.
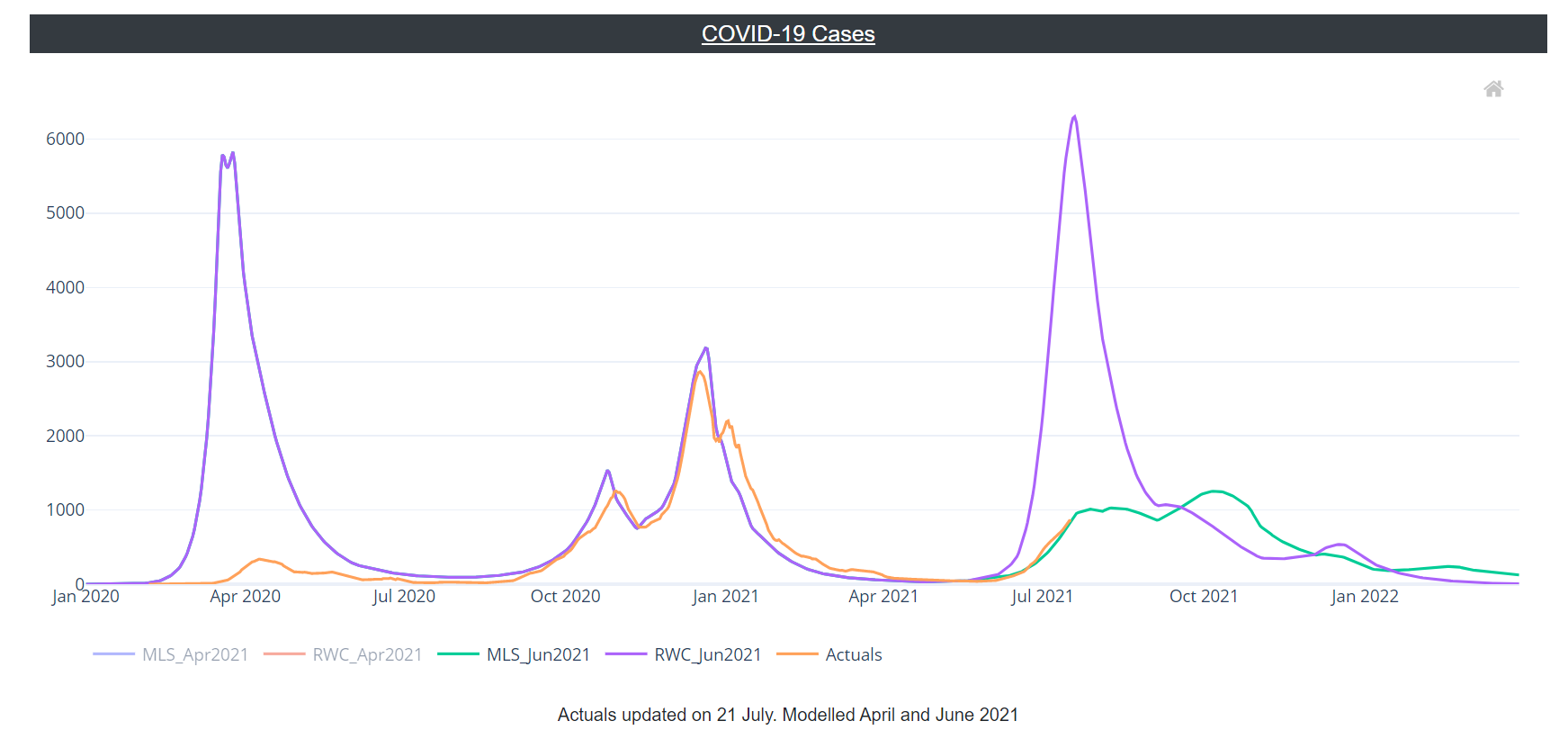
Confirmed COVID-19 cases fell between early January and early June 2021 but have begun to rise again. At present, observed COVID-19 cases are at the level estimated by the June 2021 MLS. (Note that for the model scenarios, “Cases” refers to symptomatic cases only so may be an underestimate.)
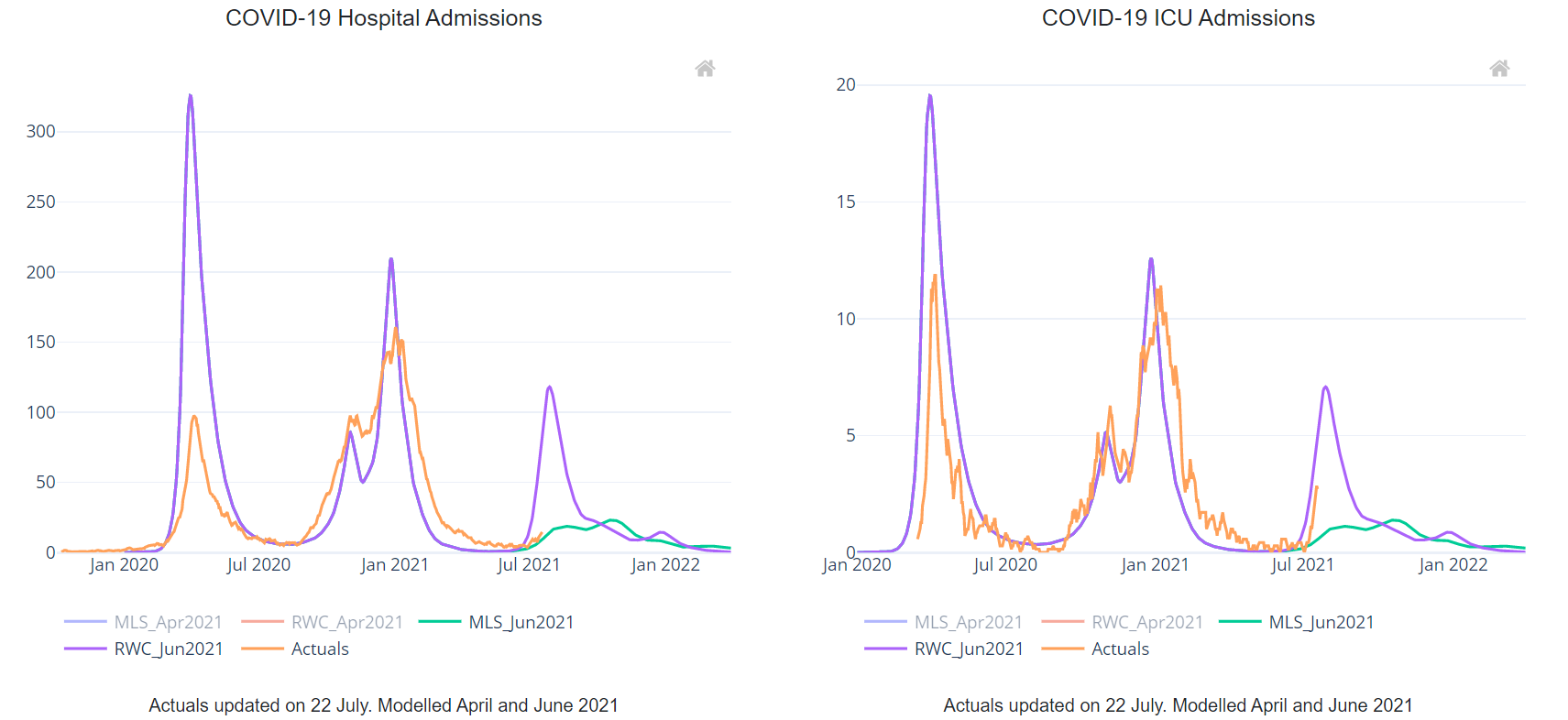
Levels of COVID-19 hospital admissions were low and stable in May and June, but hospital admissions may be showing early signs of increase in July 2021. On 18 July, the observed value of COVID-19 admissions was well below the level estimated by the June 2021 RWC scenario and slightly higher than the level estimated by the MLS. The RWC scenario suggests that there could soon be a increase in hospital admissions, but the observed data is currently closer to the MLS that suggests a slower increase in hospital admissions.
COVID-19 ICU hospital admissions have been low and stable since May. The observed value for this indicator was 2.7 admissions per day on 18 July (rolling seven day average) - below the levels estimated by the reasonable worst case (RWC), but above the level estimated by the MLS on 18 July. The trend appears to be following the sharp increase suggested by the RWC rather than the gradual curve in the MLS.
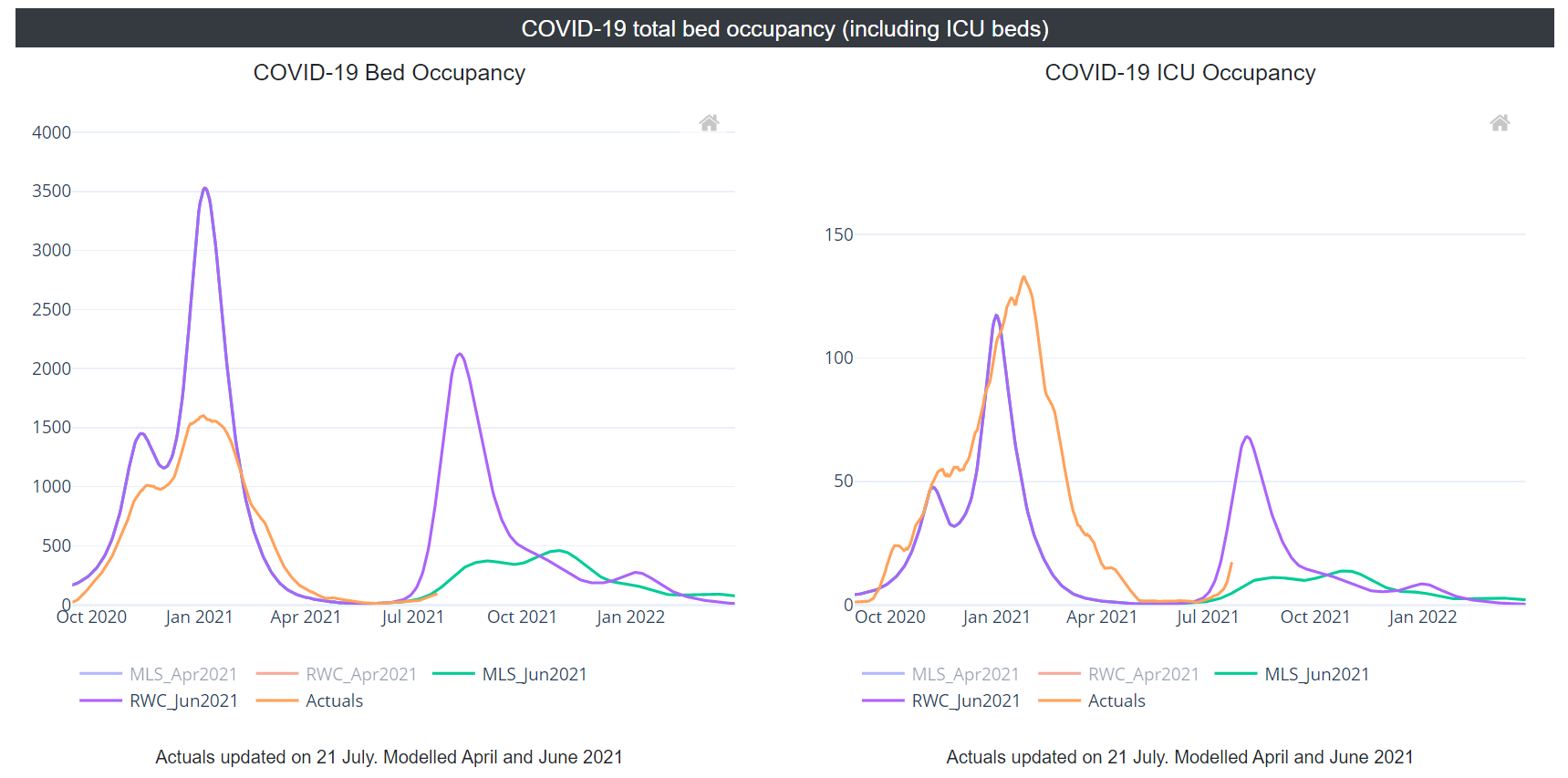
COVID-19 confirmed total bed occupancy (which includes ICU beds) decreased through January to April 2021, and has remained at low levels since May. As of 21 July 2021, COVID-19 confirmed total bed occupancy was a little below the level estimated by the MLS.
COVID-19 confirmed ICU occupancy has fallen since peaking on 24 January 2021. Since its peak, ICU occupancy fell at a steady rate until the end of April and was relatively stable in May and June 2021, but may be showing signs of increase in July 2021. As of 21 July, the current level of COVID-19 confirmed ICU occupancy was above the level estimated by the MLS but below the RWC.
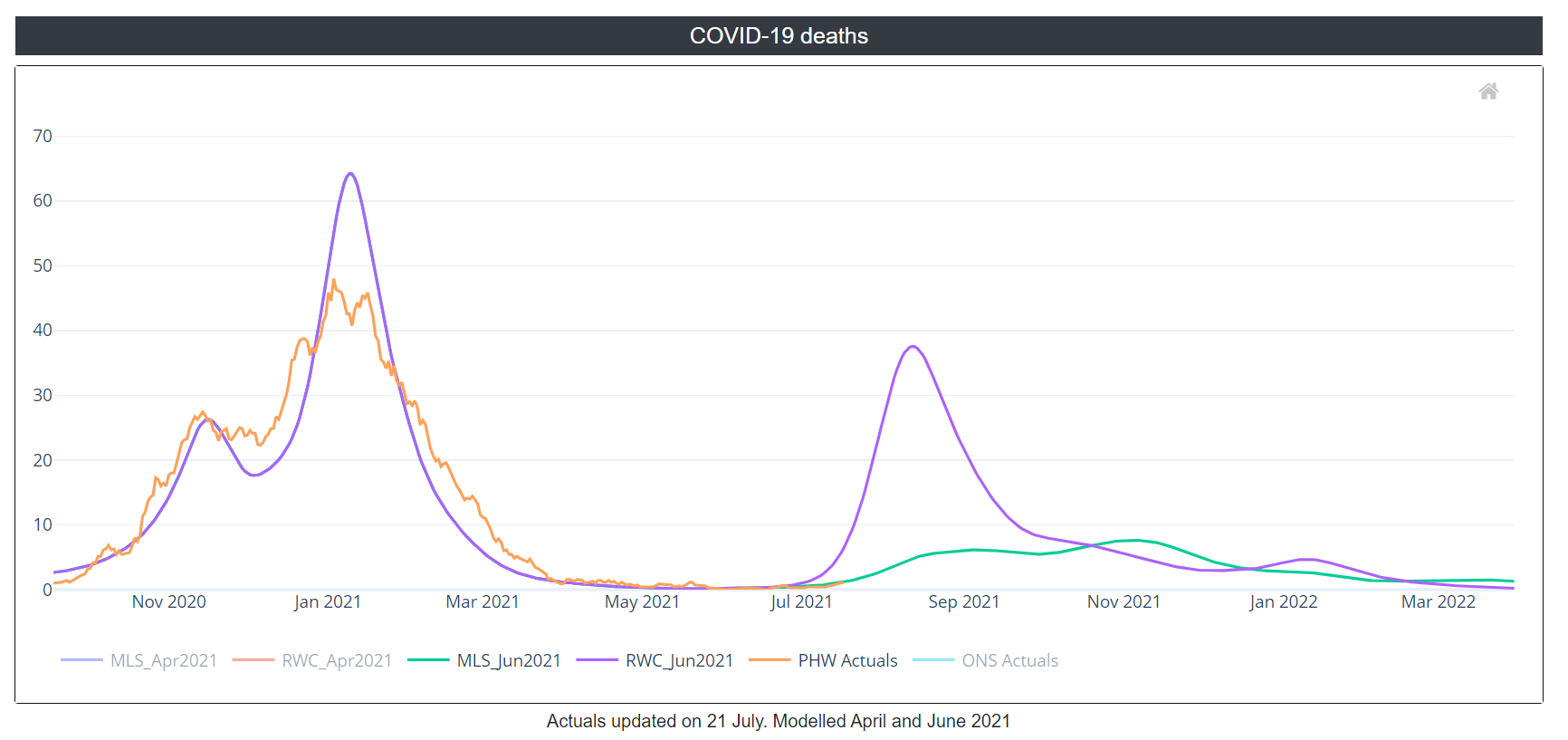
COVID-19 deaths fell from mid-January to late March and have been stable at a low level since April. The current death rate on 17 July (source: PHW) is at the level estimated by the MLS at just over 1 death per day. (Note that the RWC and MLS scenarios use the ONS COVID-19 Registered Deaths source to model their estimates.)
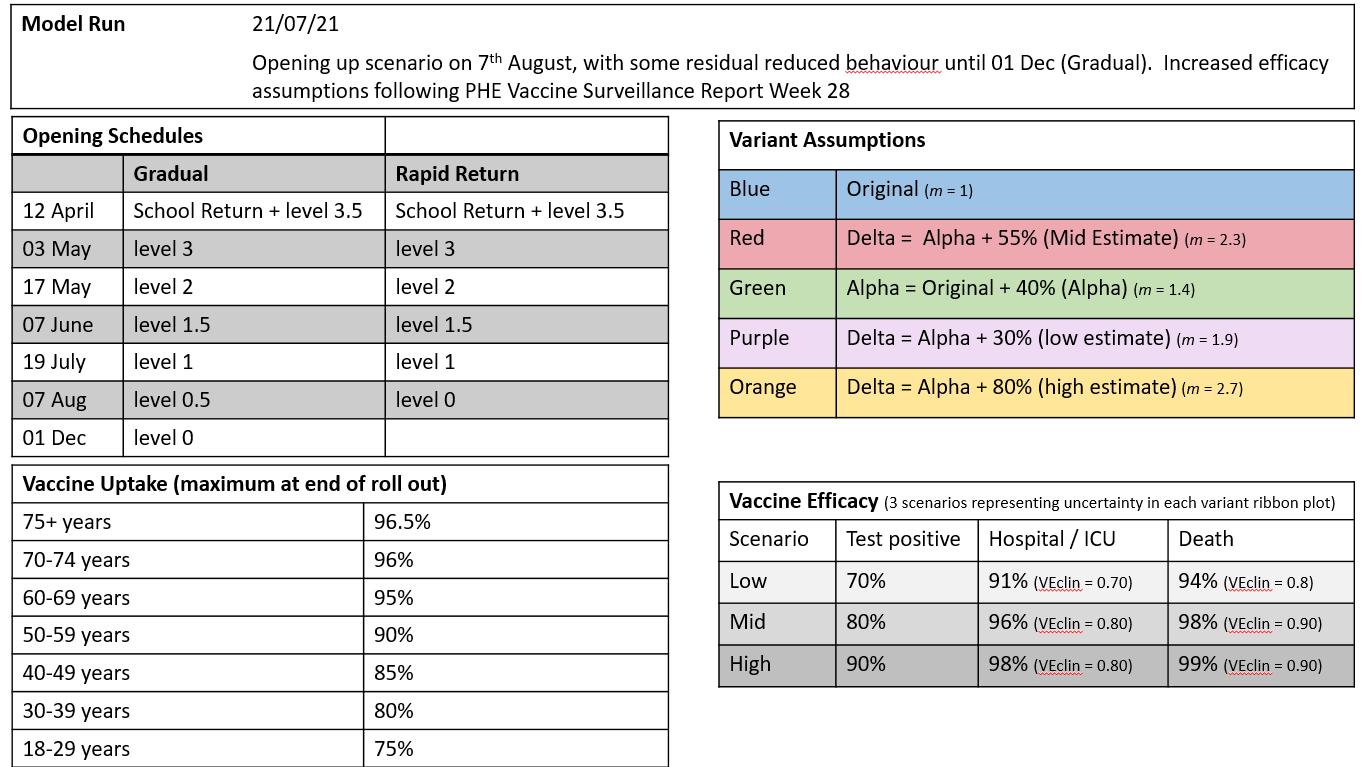
Swansea University Modelling 22 July
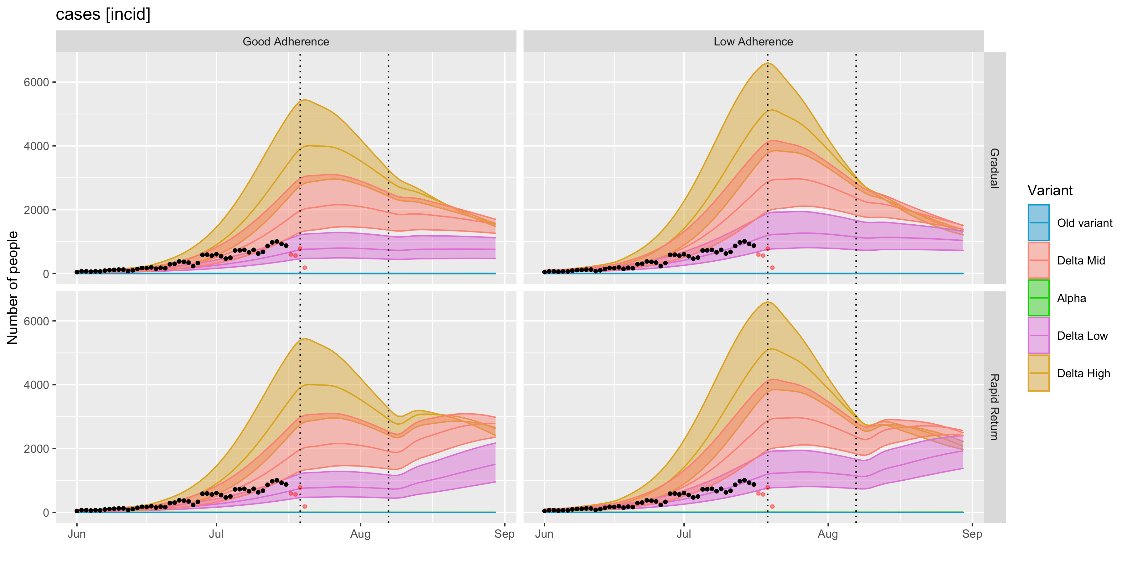
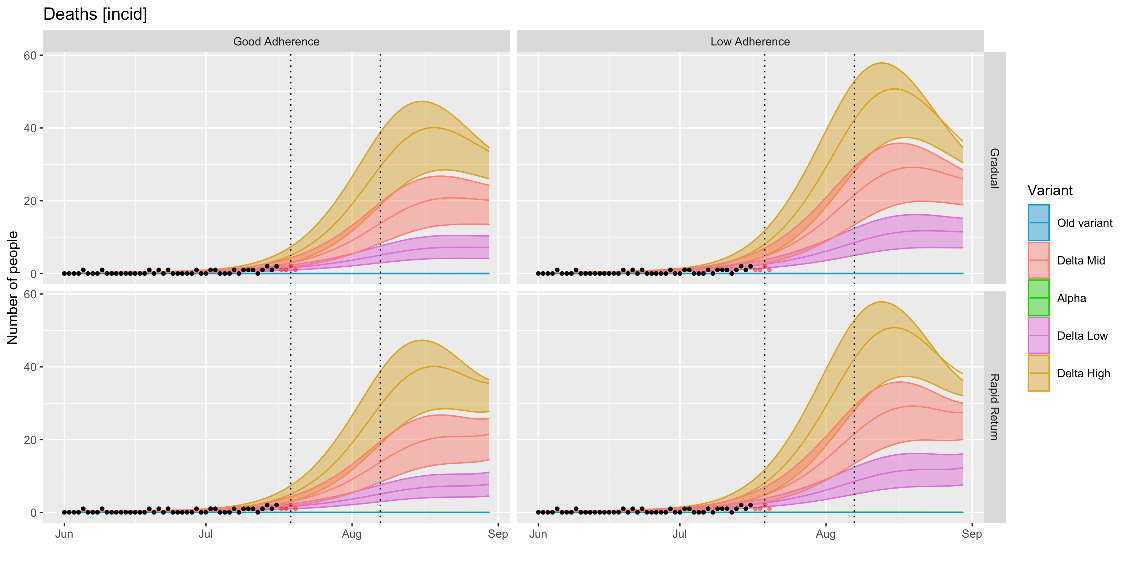
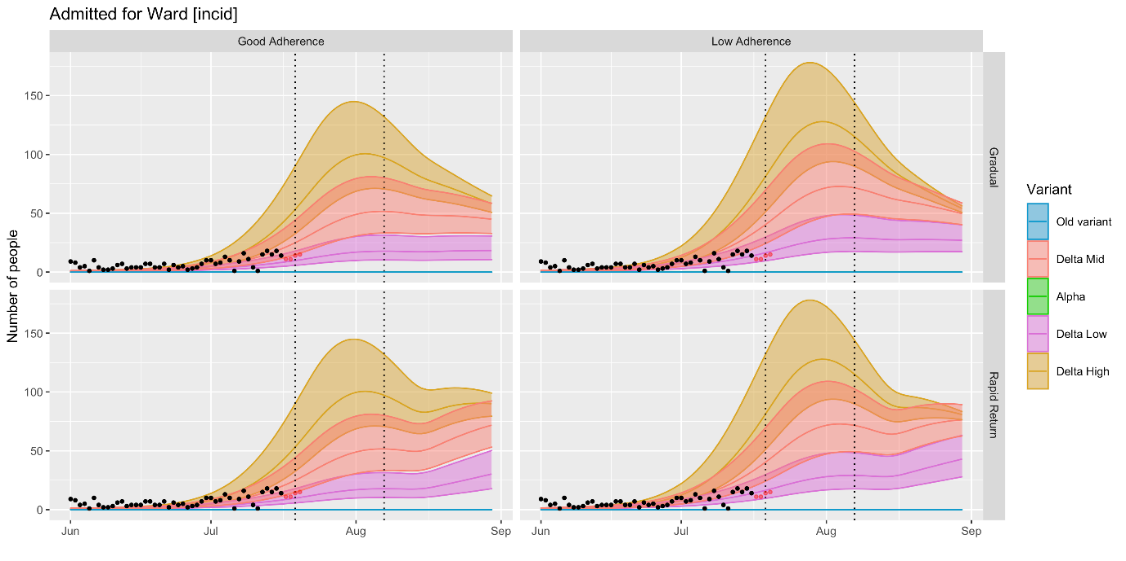
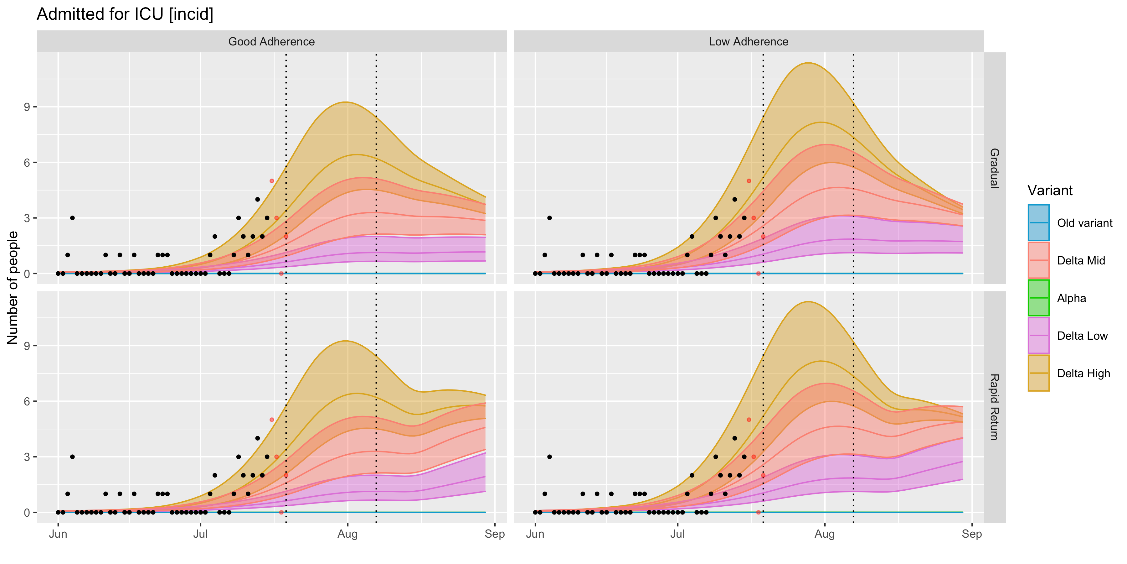
The modelling published on 12 July has now been updated with new vaccine rollout data, less optimistic assumptions on vaccine uptake in the young, a mid-estimate of delta transmissibility and the latest vaccine efficacy published by Public Health England.
Two opening scenarios are also included- one in which contacts return to pre-pandemic levels on 7 August (rapid return) and another in which ongoing protective behaviours delay this return until 1 December (gradual). The results highlight the importance of encouraging a baseline level of population protective behaviours at this stage in the pandemic, despite the excellent progress of the vaccination programme. SAGE have previously considered the need for baseline measures and sustaining behaviours beyond the lifting of non-pharmaceutical interventions:
- SPI-B: Sustaining behaviours to reduce SARS-CoV-2 transmission, 30 April 2021
- EMG, SPI-M and SPI-B: Considerations in implementing long-term ‘baseline’ NPIs, 22 April 2021
Assumptions
Results
Cases are currently tracking with the lower estimates of ‘delta-mid’ or the upper-end of ‘delta low’. Current modelling suggests that cases could soon begin to plateau, partly as a result of reduced contact networks during the school break, although if all baseline population protective behaviours were to end following the 7 August announcement modelling (rapid return scenario) estimates a subsequent increase in cases, deaths and hospitalisation.
Note that even once all non-pharmaceutical interventions are lifted it is likely that some level of population-level behaviours will remain for a period, so the ‘rapid return’ scenario should be interpreted as a hypothetical worst case rather than a realistic scenario, although there is considerable uncertainty around population behaviours in the longer term and the impact of factors such as waning immunity and the risk of novel variants of concern.
COVID-19 Evidence Centre: Rapid review on the impact of the COVID-19 pandemic on the mental health of health and social care workers within the UK
Health and social care workers may be at risk of developing negative mental health outcomes due to their roles in providing care to patients with COVID-19 (Shaukat et al. 2020). A literature search was conducted by the Wales COVID-19 Evidence Centre in May 2021 to summarise the evidence from primary studies reporting on the mental health of health and social care workers (HSCWs) in UK settings during the COVID-19 pandemic.
The evidence is limited to 20 cross-sectional studies; half were UK-wide, but none were specifically from Wales. The studies provide a snapshot of mental health outcomes at the time of the surveys but are susceptible to selection and recall bias and do not show causative effects. Most studies were during or following the first wave of COVID-19. One study was repeated in the second wave.
Evidence of Impact
A wide range of prevalence rates of anxiety (16-47%), depression (15-47%), PTSD (15-40%), Stress (28-45%), and Burnout (19-75%) was self-reported, generally using validated scales, for health and social care workers in the UK, predominantly in the first wave. Other outcomes include poor concentration (60%), insomnia (52%), mental health decline (47%) and ‘disorder’ (45%), problem drinking (7%) and a wide range of prevalence of distress (1-92%).
There was a limited number of studies which involved social care workers. A single study of specifically social care workers reported high rates of increased depression (60%) and increased tension (81%).
Policy Implications
The evidence from 20 cross-sectional UK studies conducted predominantly in the first wave of the pandemic suggests that there was a substantial adverse impact on the mental health of health and social care workers at that time.
Whilst the proportion of the workforce affected may be over-estimated by the study designs available, it is likely to be significant enough to warrant availability of mental health support to staff being a priority.
Currently, risk factors such as female staff members, with a pre-existing or prior mental health disorder and having worries about COVID-19 transmission/ PPE could be used to identify staff most at risk for support.
Few data were reported on the mental health of HSCWs in ethnic minority groups: two studies of NHS trust staff and GPs in Leicestershire had majority or total sample of ethnic minority respondents. Findings were not dissimilar to studies with predominantly white respondents.
Currently the confidence in the strength of evidence is low (cross-sectional studies) owing to limitations and bias of surveys compared to more rigorous study designs. Further research, including actively monitoring and collecting data from health and social care staff, is needed to understand the longer-term mental health impact and the severity of and risk factors for those impacts.
Full paper to be published shortly.
ONS: Coronavirus and the social impacts of ‘long COVID’ on people’s lives in Great Britain: 7 April to 13 June 2021
The ONS has published the results of its opinions and lifestyle survey for the period 7 April to 13 June 2021, looking at the impact of the pandemic on people by their self-reported COVID-19 status. The full report is available, and a summary is provided below.
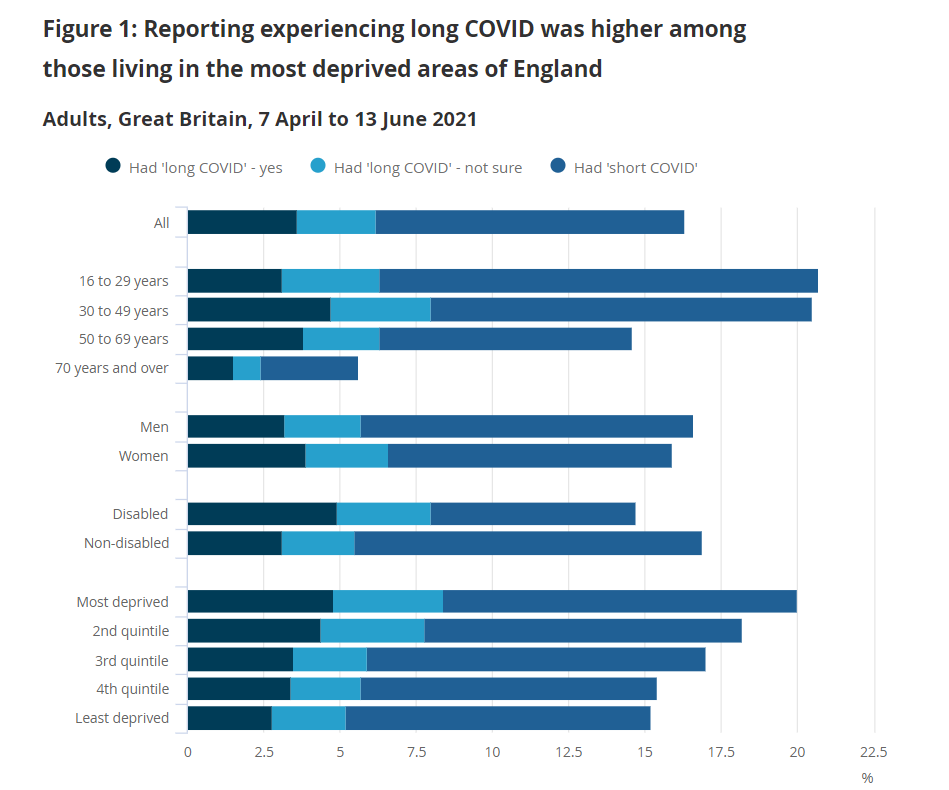
Over the period 7 April to 13 June 2021, 6.2% of adults said they may have experienced long COVID since the start of the pandemic; this includes 3.6% who said they had experienced long COVID, and 2.6% who said they were unsure if they had experienced long COVID; a further 10.1% reported they had at some point had a positive test for or believed they'd had coronavirus (COVID-19) but had not experienced long COVID.
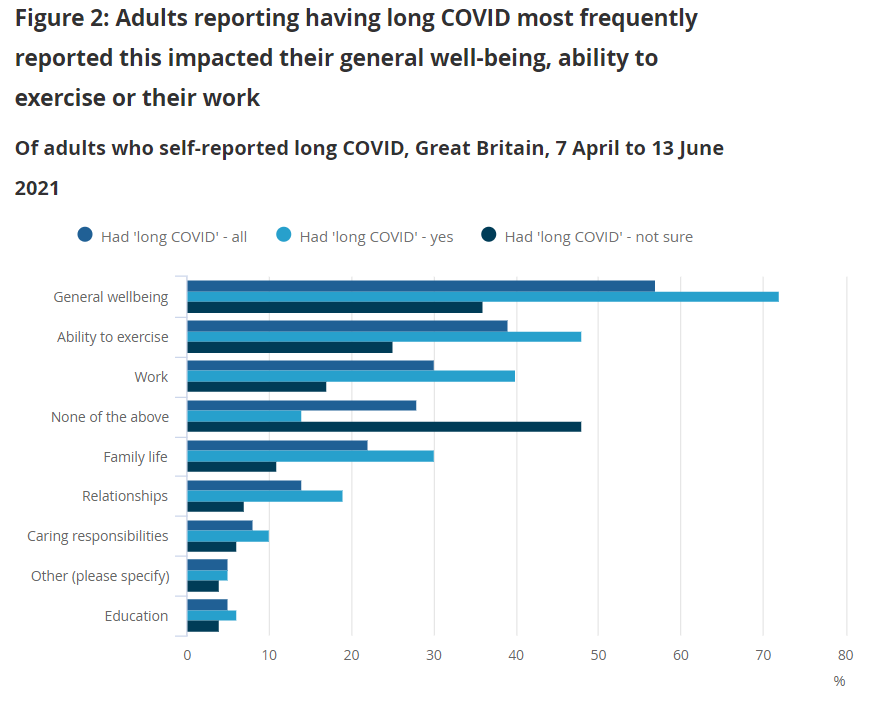
Almost 6 in 10 (57%) of those who may have experienced long COVID reported this had negatively affected their general well-being; around 4 in 10 (39%) reported it had negatively affected their ability to exercise and 3 in 10 (30%) reported it had negatively affected their work.
Of those who may have experienced long COVID, personal well-being levels across all four personal well-being indicators were lower compared with those who reported they'd not had COVID-19 (in any form); anxiety (4.6 for long COVID, 3.8 for not had COVID-19), life satisfaction (6.4 for long COVID, 7.1 for not had COVID-19), feeling that the things done in life were worthwhile (6.9 for long COVID, 7.4 for not had COVID-19) and happiness (6.5 for long COVID, 7.1 for not had COVID-19).
Of those who may have experienced long COVID, 3 in 10 (30%) reported experiencing moderate to severe depressive symptoms in the last 2 weeks compared with 16% of those who had not had COVID-19; a quarter (25%) were likely to have some form of anxiety compared with 15% of those who had not had COVID.
Nearly 1 in 2 (44%) of working adults who may have experienced long COVID reported that their work had been affected by the coronavirus pandemic, compared with around 1 in 3 (36%) among working adults who had not had COVID-19.
Of those who may have experienced long COVID, almost a quarter (22%) reported their household finances had been affected by the pandemic compared with 13% of those who had not had COVID-19.
Self-reporting of experience long COVID was higher among those living in areas of higher deprivation, reflecting similar trends from the Coronavirus Infection Survey which found that long COVID prevalence was highest in people aged 35 to 69 years, females, people living in the most deprived areas, those working in health or social care, and those with another activity-limiting health condition or disability, although this may not be attributable to cause and effect relationships.
Public Health England variant reports
Public Health England has published its most recent risk assessment of the delta variant. Immunity after natural infection has now been upgraded from amber to red status, following evidence of an increased risk of reinfection for delta compared with Alpha, although this is with low confidence due to small numbers.
A risk assessment of Beta is also included, although currently Beta is largely being outcompeted in countries where Delta is prevalent. This reflects new data that suggests Beta is less fit than Alpha but may have a higher rate of re-infection.
The most recent Technical Briefing (19) has also been published, which looks at national surveillance of infections in more detail. Of the 93,197 people who tested positive between 12 April and 27 June 2021 98.8% were in people who have never had COVID-19, with 980 possible reinfection events.
86% of Delta cases in England are currently occurring in people with no previous infection or who have not been fully vaccinated, supporting the need to encourage as many of the population to get double vaccinated as possible.
New data from the SARS-CoV-2 Immunity and Reinfection Evaluation (SIREN) study, looking at a cohort of 44,000 regularly tested NHS staff, shows an uptick in test positivity in this cohort in July to 0.54% tested between 28 June and 11 July compared to 0.01% between 17 and 30 May.
Of the 263 SIREN participants with a positive test, 221 (84%) occurred 14 days or more after their second vaccine dose. Since April 2021 there have been 51 potential reinfection events, 3 of which were at least 21 days after the first vaccine dose and 42 (82%) were at least 14 days after the second vaccine dose.
AMS Preparing for Winter 2021/2022 report
Following a request from the UK Government Chief Scientific Advisor on behalf of SAGE, the Academy of Medical Sciences has published the follow up to its 2020/21 paper, in order to: explore the health and social cared challenges presented by winter 2021/22; develop a range of scenarios; identify priority areas for government action; determine future research needs and consider the transition towards reducing population transmission of COVID-19. Read the full report.
The report, which is comprehensive and makes a number of recommendations for Government action, emphasises that despite the successful vaccination campaign and easing of restrictions across the UK the pandemic is not over. It highlights several key priorities for the winter:
- Maximising the speed and uptake of vaccination in all eligible age groups and preparing for possible booster vaccines for COVID-19 and influenza later in the year; including consideration of effective communication and engagement strategies to engage population groups with low coverage, typically in areas of deprivation. Vaccine coverage should be maximised in key groups such as health care workers and prospective higher education students.
- Consideration should be given by the Joint Committee on Vaccination and Immunisation around the possibility of vaccinating school aged children against COVID-19, considering the balance of risks and benefits and ethical issues involved with this.
- Supporting people’s ability to self-isolate on receipt of a positive test through financial, emotional, informational, practical and social support, particularly focusing on the lowest socio-economic groups. Provision of access to fast and accurate test and trace systems that also limit unnecessary isolation is also important.
- Boosting NHS capacity to build resilience against future outbreaks of COVID-19 as well as other infectious diseases by improving infection prevention control, making environmental interventions or upgrades and increasing testing capacity in order to begin dealing with the backlog of non-COVID care.
- Providing clear guidance for environmental and behavioural precautions to empower individuals and organisations to protect themselves and others, particularly those most vulnerable from infection. The use of measures such as face coverings, physical distancing and working from home should continue to be recommended where the risk of transmission is high.
The report also outlines three key challenges that will be faced by the UK this winter and beyond:
- A resurgence of respiratory diseases such as Respiratory Syncytial Virus (RSV) and influenza in addition to COVID-19. Although mortality may be less severe than the previous winter a rise in infections will still place considerable pressure on the health service and also lead to higher levels of long COVID. It is estimated that outbreaks of RSV in the autumn and influenza in the winter could be between 1.5 and 2.2 times the magnitude of usual levels and could overlap with a peak in COVID-19 infections, placing additional pressure on primary and secondary care.
- Wider health and wellbeing impacts of the pandemic, such as long COVID, mental and physical deconditioning and the impact of delays in diagnosis and disease management during the pandemic. It is anticipated that non-communicable diseases such as asthma, chronic obstructive pulmonary disease and others are likely to be exacerbated over the winter period.
- Continued disruption to health and social care deliver including managing the backlog of treatment and diagnosis built up over the pandemic, incorporating infection prevention measures and the financial precariousness of social care, including the risk of staff burnout and fatigue compounding issues of staff capacity and vacancies.
In addition the report highlights uncertainties around the duration of post-vaccination immunity in different groups, the possibility of additional variants of concern that may have greater vaccine escape.
The Technical Advisory Group are drafting a paper to reflect on the issues raised in the AMS report from a Wales perspective and to make recommendations relevant to Winter 21/22.
The full paper is available on the Academy of Medical Sciences website.
Royal Academy of Engineering – Infection Resilience Environments
A report commissioned by the UK Chief Scientific Advisory on behalf of SAGE has been published by the Royal Academy of Engineering, supported by its partners in the National Engineering Policy Centre. They were asked to consider:
- How we can redesign and retrofit buildings and transport to make them more resilient to the spread of infection in future; and
- What should be done ahead of winter 2021/2 to operate buildings and transport in a way that reduces the risk of COVID-19 transmission, and makes them acceptably safe while enabling a degree of normality.
The report describes an urgent need to monitor and improve the ventilation in public buildings, as well as improving industry knowledge and skills to reduce the impact of COVID-19 and other public health issues. The report underlines the fact that while adequate ventilation standards are already covered by existing building regulations, however implementation is often poor as a result of lack of awareness, understanding and skills. If not addressed, it is predicted these flaws could disrupt management of the COVID-19 pandemic and future public health emergencies. Investment in research and development is also needed to clarify knowledge gaps such as acceptable minimum standards for ventilation, to manage infection risk and underwrite regulation and enforcement. It is also emphasised that taking these steps need not compromise the UKs Net Zero policy and both movements should be integrated to consider both energy-use and infection control.
The full paper is available on the Royal Academy of Engineering website.
Published papers from SAGE 22 July 2021
SPI-M-O: statement on their concerns for next few months
Members of SPI-M were asked to provide a paper on what was concerning them in the current months to present to SAGE.
As the final step of easing restrictions of the Roadmap is taken, it is expected there will be further waves of infections, hospitalisations, and deaths, as discussed in SPI-M-O’s latest modelling of the potential impact of Step 4. One key concern for SPI-M-O is that any epidemic trajectory that could lead to unsustainable pressure on the NHS or other adverse outcomes would need to be identified and a contingency of stringent measures enacted in an extremely short time period in order to be avoided. The lagged nature of the pandemic also means that a doubling in hospitalisations is likely to happen even if action to prevent new infections is taken and delaying introduction of measures increases the risk that measures will need to be more stringent when applied.
There is also a risk that with high numbers of cases, testing capacity could be overwhelmed, hampering surveillance efforts, the ability to rapidly detect new variants of concern. Testing may also be impacted by changes in testing behaviour in the general population, as apps stop being used or testing take-up reduces. The impact of high prevalence on workforce preparedness and critical infrastructure if a large number of people are required to isolate is also a concern.
High community prevalence will be a particular challenge for hospitals and care homes, which are known to be more risk settings. Immunocompromised and more vulnerable people are more likely to come into contact with the health and care system. Higher prevalence will also increase the number and strength of challenges from COVID-19 that vaccinated individuals will face- leading to a possible recalculation against a vaccine effectiveness previously estimated during a period of low prevalence.
There may also be other populations, such as those not registered with the health system, where SARS-CoV-2 infections are spreading but not identified; these may propagate and continue increases in the wider population. If those who remain unvaccinated are focused in higher risk groups, such as Black, Asian, and minority ethnic individuals or those living in urban or higher transmission settings, it is possible that there will be more and more serious health outcomes, amplifying the inequalities already present.
With spatial heterogeneity in population immunity, it is possible that some areas may have significant further growth in cases and hospitalisations, even after others have peaked and incidence is clearly decreasing. These effects on healthcare may be exacerbated by differential provision in different locations, for example, some places may have more cases and smaller hospitals.
Waning immunity to vaccination and infection-acquired immunity and reduced cross-protection to novel variants are a significant concern, given that control measures are likely to rely on population immunity effects. This, however, is unlikely to be important until later in the year, and into 2022.
SPI-M-O is concerned that September and October 2021 will be a particularly risky point in the trajectory of the epidemic. It is likely behaviours will take time to return to more normal levels and, if this coincides with the return of schools and universities in the autumn, significant pressures on healthcare could be seen. This could be exacerbated by other normally seasonal infectious diseases increasing in prevalence.
During the past 18 months, diseases such as influenza, Respiratory Syncytial Virus (RSV), and norovirus, have been circulating much less in the population than previous years. Their transmission dynamics have changed due to the measures to control COVID-19 and, as a result, there may be a period of unpredictable epidemics of these diseases before their normal seasonal patterns return3. It is also possible there will be interactions between SARS-CoV-2 and other infections, both in combination and in competition. Any such effects are as yet unknown. Surveillance of COVID-19 may also be more difficult during peaks of other respiratory viruses.
Increasing numbers of infections combined with selection pressure from vaccination (either one or two doses) may create an environment for further viral evolution. This combination may lead the virus evolving in a way that escapes immunity, however, it will be very difficult to predict any precise genetic changes. Excellent surveillance systems are needed to ensure any novel variants are identified.
If a novel variant emerges and successfully establishes itself, options for intervention may be even more limited. A novel variant would be of concern if it has i) a transmission advantage; ii) escape from immunity (vaccine- or natural infection-induced); or iii) leads to more severe health outcomes, or any combination of these three.
Rapid identification of genetic variants remains crucial. The monitoring the emergence and spread of the alpha and delta variants was possible due to the S-gene target failure signals. Further data streams from rapid typing are vital, and it is essential for these to be linked to epidemiological patterns to identify potential outbreaks and establishments of new or imported variants.
The international context of the pandemic will remain important as the UK epidemic is not happening in isolation. Global surveillance, particularly on the emergency of and control of novel variants of concern, and vaccination is required to bring infections worldwide under control. Any increase in foreign travel over the summer and the return of international students to universities in the autumn is of particular concern.
The full paper is available on the GOV.UK SAGE webpage.
SAGE report on Long COVID
This report includes information from ongoing studies investigating long COVID including the COVID-19 Longitudinal Health and Wellbeing National Core Study-CONVALESCENCE Study, REACT-2, PHOSP-COVID, ONS’s COVID-19 Infection Survey (CIS) and the COVID Symptom Study App.
At this stage the authors are able to answer questions on the definition of long COVID, prevalence, demographics, risk to children, impact of vaccines and risk factors.
Long COVID symptom prevalence at 12 weeks post SARS-CoV-2 infection is uncertain and estimates vary by study design, ranging from 2.3%-37% in those infected. The proportion reporting symptoms limiting daily living range from 1.2% in young adults, to 4.8% in middle age. Trends in long COVID lag but map to those for COVID-19 infections. Fatigue is the most frequently reported persistent long COVID symptom.
No clear individual syndromes have yet been identified. Consistent risk factors across studies include increasing age, female sex, overweight/obesity, pre-existing asthma, pre-pandemic poor physical and mental health, and hospitalisation for initial infection.
Evidence of long COVID prevalence specifically in school-aged children is limited and existing studies are small; published estimates suggest that it does occur but is uncommon, 25 (1.8%) of 1,379 children (all ages) experienced symptoms for ≥56 days.
Risk of Long COVID may be reduced by half in individuals who become infected after double vaccination compared to those not vaccinated; however, published evidence is limited to small observational studies, which may be subject to bias and so caution is recommended with regards to overstating the benefits of vaccination, particularly when JCVI guidance is that children are not vaccinated.
Rates of medium-long term multi-organ sequelae (respiratory disease, major adverse cardiovascular event, diabetes, renal failure, and liver disease) are elevated in patients hospitalised with COVID-19 compared with matched general population but are similar to those hospitalised with pneumonia; however, estimates of the incidence of post-infection adverse events in non-hospitalised COVID-19 cases are lacking and this will be the subject of subsequent analysis over the next few months.
The full paper is available on the gov.uk SAGE webpage.
Waning of vaccine immunity
It is highly likely that vaccine induced immunity to SARS-CoV-2 infection, and potentially severe disease (but probably to a lesser extent) will wane over time.
This is likely to be first detected by vaccine failures in vulnerable cohorts (for example a high rate of infections in people vaccinated over time, including hospitalized cases).
It is therefore likely that there will be vaccination campaigns against SARS-CoV-2 for many years to come, but currently we do not know what the optimal required frequency for re-vaccination will be to protect the vulnerable from COVID disease.
Different vaccines may induce different sorts of immunity, which may have different duration. Absolute correlates of protection are yet to be determined, but the only ready measure that can be used at scale is of serum antibody.
Even if antibody levels after vaccination wane to allow significant numbers of infections, this might have an effect of boosting the primed immune system of vaccinees who would experience mild or asymptomatic infections. In turn this could result in a broader immune response than expected if vaccines induced a sustained sterilizing immune response. Measurements of immune responses in persons who are infected following vaccination will be important to understand this.
Current studies (PHE and National core studies) have assembled longitudinal cohorts but are only funded or planned to continue for 12-18 months, and waning may be important in the time frame of 2-5 years. There is a need to decide what further longitudinal studies are required, and to what extent they can build on existing funded studies which could be extended, or whether de novo studies will be needed.
We strongly recommend that funding is maintained to allow some of the current cohorts to be followed for longer times periods, and to included subsets who remain unboosted.
Maintaining focussed studies with cohorts of individuals in whom waning may happen sooner are particularly important since these groups may act as ‘canaries’ in signalling the time point beyond which waning vaccine immunity might become an issue. It will be important to relate immunological information to parallel studies of disease outcome, particularly those for severe disease.
These studies should continue to include a collaboration of public health, academia and clinical scientists working together with support for the appropriate data linkage, to measure VE in the real world and to understand mechanisms of protection and waning.
The full paper is available on the gov.uk SAGE webpage.
Long term evolution of SARS-CoV-2-NERVTAG
The emergence of new variants of SARS-CoV-2 is related to the amount of circulating and transmitting virus (almost certain), i.e. higher transmission translates to a higher risk of variants of concern. Reducing viral load both nationally and globally will reduce the frequency and number of new variants arising (highly likely).
Although Current or future vaccines should be effective against all variants (highly likely), new variants may result in increased morbidity and mortality (realistic possibility).
Current variants have similar outcomes (high confidence).
Using anti-viral drugs irresponsibly will result in resistant variants (almost certain).
This paper assesses four hypothetical scenarios by which SARS-CoV-2 could further evolve and acquire, through mutation, phenotypes of concern, according to likelihood, impact and possible mitigations. For this purpose, we consider mutations in the ‘body’ of the virus (the viral genes that are expressed in infected cells and control replication and cell response), that might affect virus fitness and disease severity, separately from mutations in the spike glycoprotein that might affect virus transmission and antibody escape.
The four scenarios considered are:
- variant that causes severe disease in a greater proportion of the population than has occurred to date.
- a variant that evades current vaccines.
- a dominant variant that evades current anti-viral strategies
- SARS-CoV-2 follows an evolutionary trajectory with decreased virulence
The full paper is available on the gov.uk SAGE webpage.
International vaccination: potential impact on viral evolution and UK public health
This paper builds on previous SAGE discussions on border and travel restrictions – including consideration for the importation of novel variants.
The biggest threat to the UK’s health security and response to the SARS-CoV-2 pandemic is the emergence (and establishment within the UK) of variants that either have increased transmissibility, increased disease severity, escape prior immunity, or a combination of these characteristics [high confidence]
Substantial global circulation of SARS-CoV-2 will lead to the evolution of new variants and continued risk of importation to the UK [medium confidence]. Increased international vaccination by donation/sharing of purchased doses, or supporting increased manufacture, has the potential to reduce the appearance and establishment of variants internationally, as well as the risk of their importation to the UK [medium confidence].
If immunocompromised or populations otherwise vulnerable to chronic infections are shown to be a significant source of new variants with concerning characteristics, then focussing global vaccination efforts to these populations (and their contacts) may reduce the risk of new variants of concern emerging [medium-high confidence].
Risk of importation of novel variants
As the number of travellers to the UK increases so will the risk of importation of variants and the burden on genomic surveillance systems [high confidence]. The number of importations that would result in the establishment of local transmission of a new variant is difficult to predict due to over-dispersion and the unpredictability of variant characteristics such as transmissibility [high confidence]. Border measures are likely to delay but not prevent introduction [high confidence].
If vaccination continues to protect against infection, and reduce onward transmission, then requiring travellers to be vaccinated is likely to reduce the risk of importation but may exacerbate inequalities if international vaccination coverage remains low and heterogenous [high confidence].
Imported cases are less likely to lead to outbreaks and established community transmission in the UK if transmission in the UK is controlled, by population immunity or non-pharmaceutical interventions [high confidence].
It is unclear which domestic communities may be at higher risk from imported variants. Increasing domestic vaccination in all groups or those with higher exposure to international travellers is likely to reduce the probability of establishment of transmission after importation [high confidence].
Benefits of international vaccination
A successful domestic strategy hinges on achieving low numbers of infections globally to reduce the emergence of novel variants of concern [medium-high confidence].
Establishing the optimal priority or targeting of international vaccination efforts is complicated by biological uncertainties and logistical complexities (e.g. distribution, vaccine hesitancy, regional stability, etc). In the short term, prioritisation of countries with higher volumes of travellers coming to or from the UK (or for whom more open borders are economically desirable) could be considered [low confidence].
Multilateral cooperation and a commitment to increasing global vaccination rates, in part by sharing resources such as doses, is highly likely to have the biggest impact on the incidence of infections globally and thus the biggest impact on the risk of the emergence of new variants [medium-high confidence].
It is unknown how levels of vaccination change the relative risk of the appearance and establishment of an immune escape variant. Most current variants of concern emerged before mass vaccination or high population immunity from infection [medium confidence]. Any level of population immunity may increase selection pressure for immune escape variants but there is no evidence to suggest this pressure would be greater for vaccine-induced immunity than immunity driven by infection [medium confidence].
The full paper is available on the gov.uk SAGE webpage.
